Phosphorus Control in ESKD – Owning Your Numbers and Optimizing Outcomes.
Why Phosphorus Matters More Than You Think
When you’re living with kidney failure, there’s a lot to juggle—appointments, fluid balance, dialysis sessions, lab numbers. It can feel overwhelming. But one piece of your care deserves special attention because it’s one of the few things you can directly influence day to day: your phosphorus level.
Phosphorus isn’t just “another number.” In end-stage kidney disease (ESKD), phosphorus control in ESKD plays a major role in your overall outcomes:
- It affects your bones, heart, blood vessels, and energy level
- It contributes to elevated PTH and calcium imbalance
- And—most importantly—it’s something the dialysis machine can’t fix on its own
Many patients are surprised to learn that even with regular dialysis, excess phosphorus can remain in the body. Dialysis removes only some of it—not enough to reach target levels on its own. That’s where your actions—what you eat, when you take your binders, and how you approach your routine—become the difference-makers.
This isn’t about blame or discipline. It’s about opportunity. Mastering phosphorus control in ESKD isn’t about perfection—it’s about consistency, strategy, and believing that your effort makes a real impact.
Dialysis Can’t Do It Alone
There’s a myth that dialysis is like a total reset button—that the machine “cleans everything out.” But when it comes to phosphorus, that simply isn’t true.
Phosphorus is mostly stored in your bones and cells, not your bloodstream. So during dialysis, only a fraction of your total phosphorus load is removed. That’s why even patients who never miss a treatment can still struggle with high phosphorus levels.
Let’s be clear: this isn’t your fault. But it does mean that you have power your machine doesn’t.
If you’ve ever felt discouraged by the number of pills or frustrated by confusing food labels, you’re not alone. But the truth is: you’re the most important part of phosphorus control in ESKD, not the dialyzer.
Through:
- Learning which foods are highest in hidden phosphorus
- Taking phosphate binders at the right time (with meals—not before, not after)
- Asking questions and getting support from your team
—you gain something the machine can’t offer: control. This is where phosphorus control in ESKD begins: with understanding what dialysis can and cannot do.
You’re Not Powerless—You’re the Most Important Part
There’s a reason why your care team checks your phosphorus level so often: it’s not just a lab—it’s a marker of how much control you’re able to gain over something the machine can’t remove well.
Too often, patients are made to feel burdened by the challenge of phosphorus control in ESKD—as if it’s another exhausting responsibility with little reward. But here’s the truth: phosphorus is one of the few things in your care that you can directly shape with daily actions.
Small adjustments matter. And every improvement you make sends a ripple effect through your entire body:
- Your bones feel the relief
- Your parathyroid glands stop overreacting
- Your blood vessels stay more flexible
- Your need for medications may decrease over time

Let’s be clear—this isn’t about being perfect. It’s about being informed, engaged, and supported. Your role in phosphorus control in ESKD is powerful, and it deserves more credit than it gets.
Binder Options – What’s Out There and How They Work
Phosphate binders may feel like one of the least glamorous parts of kidney care—but they’re one of the most important tools for managing phosphorus control in ESKD.
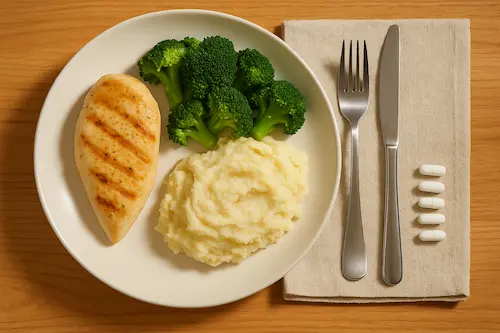
These medications work by binding to the phosphorus in your food, so your body doesn’t absorb as much. But they don’t work if taken at the wrong time. That’s why taking binders with meals is key—not 30 minutes later, and not on an empty stomach.
Here’s a simplified breakdown of the types of binders available in the U.S.:
- Calcium-based binders (e.g., calcium acetate, calcium carbonate)
Help lower phosphorus but can increase calcium; used cautiously in patients with vascular calcification risks. - Non-calcium binders (e.g., sevelamer, lanthanum)
These are calcium-free and often preferred if calcium levels are already high. - Iron-based binders (e.g., sucroferric oxyhydroxide, ferric citrate)
Help with phosphorus and may support iron levels as well.
Each binder has its pros and cons, and your doctor will tailor your prescription based on labs, tolerability, and pill burden. Understanding these options is key to successful phosphorus control in ESKD.
If you’ve ever felt binder fatigue, you’re not alone. But with proper timing and education, binders become more than pills—they become a lever you can control.
What About Xphozah? A New Option with a Different Mechanism
You may have heard of a newer phosphorus-lowering option called Xphozah (tenapanor). Unlike traditional binders that work in the gut to absorb phosphorus, Xphozah changes how your intestines absorb it in the first place.
Here’s how it’s different:
- It’s a non-binder taken orally
- It reduces phosphorus by modulating sodium-hydrogen exchange in the gut
- It works best when used with or in place of traditional binders, depending on the situation
Xphozah is an exciting option for patients who can’t tolerate multiple binders or who need another approach to reach target levels. It’s not for everyone, and it may cause diarrhea in some, but it represents a shift in how we approach phosphorus control in ESKD—away from pill piles and toward individualized treatment.
For patients with binder intolerance or persistent high phosphorus, it’s worth asking your nephrologist whether Xphozah could be part of your toolkit for phosphorus control in ESKD.
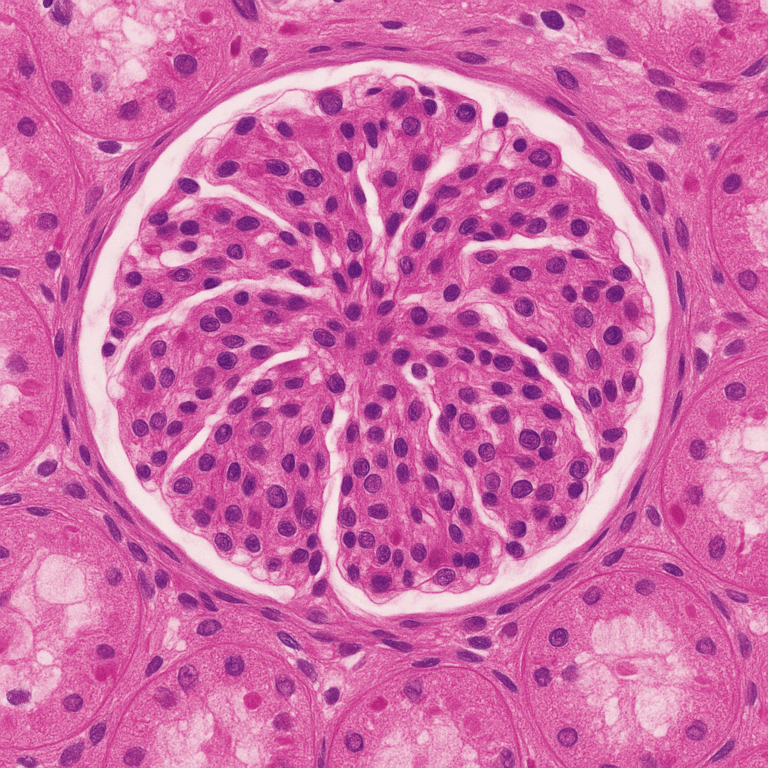
Why Bone Health Depends on Phosphorus
PhPhosphorus is deeply connected to bone health. In fact, keeping phosphorus in check is one of the most important steps ESKD patients can take to protect their skeleton.
Here’s why:
- When phosphorus builds up, your parathyroid glands release more PTH, which pulls calcium and phosphorus out of your bones
- This constant turnover weakens the bone structure and increases the risk of fractures
- Over time, it contributes to a condition called renal osteodystrophy, which makes bones fragile and painful
And here’s the kicker: most osteoporosis medications aren’t recommended for people on dialysis. That means patients with ESKD have fewer options to protect their bones once damage is done. So every opportunity to preserve bone health upfront matters.
Another issue your care team watches closely is the calcium-phosphorus product (CaXPhos)—a calculation that helps determine your risk for mineral deposits in soft tissues. When both calcium and phosphorus are elevated, the risk rises significantly. Maintaining phosphorus control in ESKD is the most important patient-dependent variable for keeping this CaXPhos down.
Think of it this way: if you mix calcium and phosphorus in a neutral solution outside the body, they start to crystallize—literally forming tiny rocks. The same thing can happen inside your arteries, joints, and skin when these levels are too high together.
If your calcium-phosphorus product gets too high, important treatments like active vitamin D analogs may have to be withheld, because they could push calcium even higher. That means your options shrink just when your body needs support the most.
This is why phosphorus control in ESKD isn’t just about labs—it’s about protecting your bones, preserving your blood vessels, and keeping the door open for therapies that your body might depend on later.
It’s a call to action: not out of fear, but out of power. You have tools. You have knowledge. And through understanding, you now have a reason to use them. To learn more about how phosphorus, PTH, and bone turnover are all connected, see our related article:
Complications of High PTH in Kidney Disease
Small Wins That Build Momentum
Sometimes phosphorus management can feel like an uphill climb. But success rarely comes from sweeping changes—it comes from consistent, sustainable actions over time.
Here are small wins that lead to big progress in phosphorus control in ESKD:
- Reading food labels to spot hidden phosphorus additives
- Taking binders with meals—not 15 minutes later
- Planning meals with your renal dietitian’s support
- Asking questions when labs change instead of feeling defeated
- Remembering that lab trends matter more than one result
Each of these actions might seem small, but together they build something bigger: momentum. And with momentum comes confidence.
You’re not working alone. You’re working with your team—your doctor, dietitian, and nurse—but you’re also leading the effort. You’re building a routine that works for you and supports consistent phosphorus control in ESKD. Download our Low Phosphorus Food Guide for Dialysis Patients to help decode labels and plan smart meals.
Final Word – You’re the Driver, Not the Passenger
Too often, people with kidney failure feel like they’re being dragged along by the disease—by appointments, machines, pills, and restrictions.
But phosphorus control in ESKD is different. This is one area where you have meaningful power, every single day.
By understanding how phosphorus works, why binders matter, and what options are available—including newer therapies like Xphozah—you step into the driver’s seat. You become the one navigating, not just following.
Perfect numbers are attainable goals. Empowered, informed decisions are the path to controlling phosphorus balance; it doesn’t have to control you.
And you’re already on the path and can achieve phosphorus control in ESKD with a combination of dietary modification and medication adherence.
Works Cited
- KDIGO 2017 Clinical Practice Guideline Update for CKD–MBD. Kidney Int Suppl. 2017;7(1):1–59.
- St Peter WL. “Management of hyperphosphatemia in CKD: emerging trends.” Clin J Am Soc Nephrol. 2015;10(3):547–553.
- U.S. FDA. Xphozah (Tenapanor) Prescribing Information
- Kalantar-Zadeh K et al. “Patient-centered approach to phosphate management in dialysis patients.” Kidney Int Suppl. 2011;79(2):123–135.