Understanding Your Labs: A Clear Guide to Creatinine, Potassium, and Beyond
Decoding the Numbers That Shape Your Care
If you’re living with chronic kidney disease (CKD), lab results are part of your regular routine. Creatinine, potassium, eGFR, BUN—it can feel like alphabet soup. You see the numbers, maybe even the red flags, but what do the labs mean?
Understanding your labs is more than just curiosity. It’s a way to:

- Track disease progression
- Detect problems early
- Understand medication changes
- Take ownership of your care
Let’s walk through the most common labs in CKD, in plain language—so you know exactly what you’re looking at, and why it matters.
Creatinine: Your Kidney’s Workload Indicator
What it is:
Creatinine is a waste product from muscle metabolism. Your kidneys filter it out of the blood. When kidneys slow down, creatinine levels go up. Both glomerular filtration and proximal tubular secretion occur within the kidney. Creatinine is exclusively eliminated by the kidneys under normal physiology, just through two different intrarenal mechanisms.
Normal range: ~0.6 to 1.3 mg/dL (can vary by lab, gender, and muscle mass)
Why it matters:
Elevated creatinine on your labs is a sign your kidneys aren’t clearing waste as efficiently. But don’t judge by this number alone—it’s affected by:
- Muscle mass (athletes may run higher)
- Hydration (dehydration falsely elevates it)
- Certain meds (like trimethoprim, fenofibrate, or biotin) can cause falsely elevated values
eGFR (Estimated Glomerular Filtration Rate): The Big Picture Number
What it is:
eGFR estimates how well your kidneys are filtering blood. It’s calculated from your creatinine, age, sex, and race. It is reported on your labs but actually measured in the blood.
CKD stages by eGFR:
- Stage 1: >90 with signs of kidney damage
- Stage 2: 60–89
- Stage 3a: 45–59
- Stage 3b: 30–44
- Stage 4: 15–29
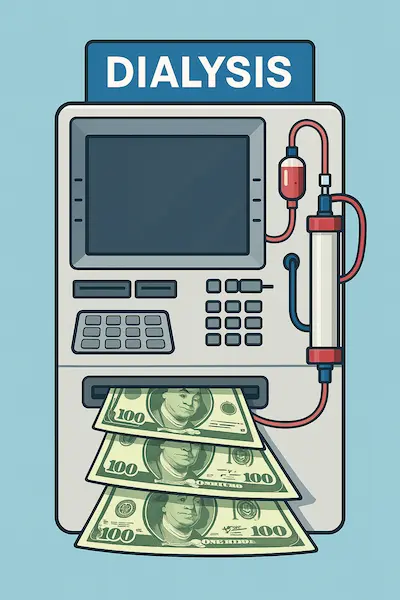
- Stage 5: <15 (may need dialysis)
Why it matters:
eGFR is the most commonly used number to monitor CKD progression. But a single low value doesn’t mean permanent damage—your provider looks at trends over time.
BUN (Blood Urea Nitrogen): A Companion to Creatinine
What it is:
BUN measures the amount of nitrogen from urea—a waste product of protein digestion—in your blood. Usually, the BUN and creatinine will go up and down in tandem. If, however, the BUN rises out of proportion to the creatinine, this can be a sign of dehydration, excessive protein intake, or something other than CKD. This drives up another calculate result on your labs called the BUN-Cr ratio which may prompt your provider to evaluate your fluid status, protein macro intake, or other work up.
Normal range: 7–20 mg/dL
Why it matters:
BUN rises with worsening kidney function, but also from:
- Dehydration
- High-protein diets
- Gastrointestinal bleeding (from digestion of red blood cells)
It’s helpful alongside creatinine, but not as reliable on its own.
Potassium (K+): The Rhythm Regulator
What it is:
Potassium is an essential mineral that helps nerves fire and muscles contract—especially the heart. Approximately 90–95% of daily potassium excretion is regulated by the kidneys, making them the primary organ responsible for potassium balance. The remaining 5–10% is lost through the gastrointestinal tract and, to a much lesser extent, through sweat and other insensible routes. This means that even small impairments in kidney function can significantly disrupt potassium homeostasis and show elevated readings on your labs.
Normal range: 3.5–5.0 mEq/L
Why it matters:
Too much potassium (hyperkalemia) can cause irregular heart rhythms, which may be life-threatening. CKD patients are at risk because the kidneys excrete potassium. Certain meds (e.g., ACE inhibitors, ARBs, potassium-sparing diuretics) can also raise levels.
Low potassium (hypokalemia) is less common but also dangerous.
Sodium (Na+): Water Balance and Volume Control
What it is:
Sodium helps regulate blood pressure and fluid balance. Sodium levels on lab tests reflect its concentration in the blood, not the total amount of sodium in the body. This concentration can be affected by changes in water balance — for example, dehydration may cause sodium levels to appear high even if total body sodium is normal. Conversely, excess water (like in heart failure or SIADH) can dilute blood sodium, making it look low despite sodium overload.
Normal range: 135–145 mEq/L
Why it matters:
Low sodium often reflects fluid overload or heart failure in CKD. High sodium may suggest dehydration or excessive salt intake. Think of sodium more as a hydration signal than a kidney marker.
Bicarbonate (CO2 or HCO₃⁻): Your Acid Buffer
What it is:
Bicarbonate helps keep your blood pH balanced. Our bodies generate acid every day as a byproduct of metabolism. It is up to your kidneys to eliminate the excess acid load. If your labs indicate the CO2 in your blood is low, it suggests that this acid load is accumulating. Bicarbonate supplements are used to buffer this acid load and reduce the burden on your remaining kidney function.
Normal range: 22–30 mmol/L
Why it matters:
Low bicarbonate (metabolic acidosis) is common in CKD and can lead to:
- Muscle breakdown
- Bone loss
- Faster CKD progression
If your level drops below 22, your doctor may prescribe sodium bicarbonate tablets or suggest diet changes.
Phosphorus & Calcium: Bone and Vessel Watchdogs
Phosphorus:
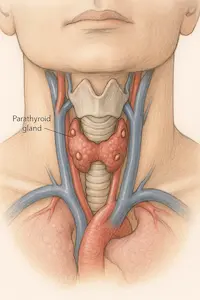
The kidneys eliminate excess phosphorus by filtering it from the blood and excreting it into the urine, maintaining a healthy balance in the body. When kidney function declines, phosphorus builds up in the bloodstream because it is no longer adequately excreted. Chronically elevated phosphorus levels trigger increased parathyroid hormone (PTH) release, which pulls calcium from bones (weakening them) and promotes calcium-phosphate deposits in blood vessels, increasing the risk of vascular stiffness and cardiovascular disease. Phosphorus can start to rise on your labs in stage 3B progressively through stage 5 when dietary restriction becomes increasingly important.
Calcium:
Calcium and phosphorus absorption in the gut is indirectly regulated by the kidneys through their control of active vitamin D (calcitriol) production. The kidneys convert inactive vitamin D into calcitriol, which then acts on the intestines to increase absorption of both calcium and phosphate. When kidney function declines, calcitriol production decreases, leading to reduced gut absorption of these minerals and contributing to imbalances such as hypocalcemia and secondary hyperparathyroidism.
These labs become more important in Stage 3b and beyond.
The Takeaway
Lab results aren’t just numbers—they’re your kidneys talking back. Understanding what each test reflects helps you partner with your care team more effectively.
So the next time your labs come in, don’t just scan for red flags. Read them like a story:
What are your kidneys saying? And what can you do in return?
References
- National Kidney Foundation. “How to Read a Comprehensive Metabolic Panel”. https://www.kidney.org
- KDIGO 2021 Clinical Practice Guideline on CKD Evaluation and Management. Kidney Int Suppl. 2021;11(1):S1–S115.