Battling Anemia in CKD: Optimizing Therapy with Individualized Targets
Understanding the Landscape of Anemia in CKD
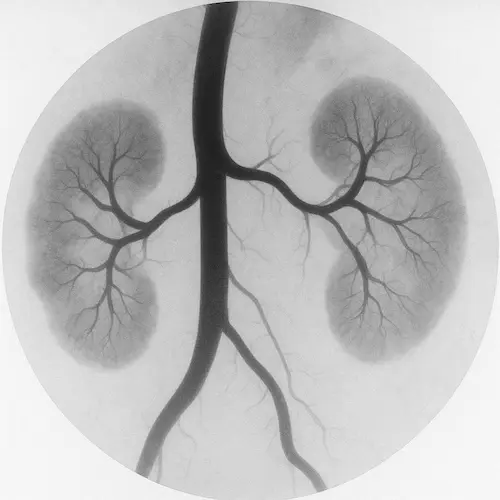
The kidneys’ decline is not a single‑lane slide; it is a cascade that changes how nearly every cell in the body functions. Among the first casualties is erythropoietin (EPO) production. As healthy nephrons disappear, the oxygen‑sensing fibroblasts that create EPO fall silent, bone marrow receives no marching orders, and anemia in CKD settles in. Patients describe a creeping exhaustion that feels nothing like ordinary fatigue. Walking the dog becomes a chore; concentrating during a business call feels like wading through syrup. Worse, the heart pumps harder against thicker blood, left‑ventricular muscle hypertrophies, and cardiovascular mortality climbs. Detecting—and treating—this complication early is therefore pivotal both for quality of life and for survival.
Root‑Cause Diagnosis: Beyond a Low Hemoglobin

Clinicians often think of anemia as “low Hb, give iron,” yet anemia in CKD demands a layered diagnostic lens because multiple factors can coexist:
- Erythropoietin deficiency – the hallmark driver.
- Absolute iron deficiency – GI bleeding, poor diet, frequent phlebotomy.
- Functional iron deficiency – ferritin appears normal but iron is trapped by hepcidin.
- Inflammatory blockade – CRP rises, ferritin is falsely elevated, TSAT falls.
- Vitamin B12 or folate depletion – less common but quickly reversible.
A concise work‑up therefore includes ferritin, TSAT, CRP, reticulocyte count, and occasionally B12/folate. The goal is to confirm that anemia in CKD is truly renal‑driven and to correct reversible contributors before escalating therapy.
Iron Repletion: Why It Comes First
Iron is the building block of hemoglobin which is the oxygen carrying molecule within the red blood cell. In anemia of CKD, adequacy of iron stores is the first order of business. While growth factors can be used to augment generation of red blood cells in the bone marrow, they will be of no use unless there are ample iron “building blocks” to form hemoglobin.
Iron may be low due to poor absorption in the GI tract, utilization for red cell production, or depletion from blood loss. Anemia in CKD exists commonly exists in a pro-inflammatory state. Co-existing conditions such as infection, hyperparathyroidism or chronic metabolic acidosis cause increase in systemic inflammation. Hepcidin is an inflammatory substance that increases in inflammation and blocks intestinal absorption of iron. Patients receiving erythrocyte stimulating agents (ESA) will have increased iron utilization for red cell production and thus increase iron demand. Depletion from blood loss usually requires additional investigation to control bleeding in addition to replacing lost iron stores.
Oral Iron—Helpful but Often Insufficient
If iron deficiency is found during workup for anemia in CKD, non‑dialysis patients may start with oral iron replacement. If side‑effects (constipation, nausea, dark stools) derail adherence, newer preparations—ferric maltol or sucrosomial iron—provide similar elemental doses with less gastric distress. Even so, diminished gut absorption in stage 4–5 CKD often stunts response.
Intravenous Iron—Reliable Restoration
If patients with anemia of CKD are intolerant to oral iron options, IV formulations bypass absorption barriers and raise hemoglobin faster. Ferric carboxymaltose 750 mg twice or iron sucrose 200 mg on five dialysis sessions can add 1–1.5 g/dL of Hb within a month. Post‑infusion checks at week 4 ensure ferritin > 300 ng/mL and TSAT > 30 %. Maintaining those thresholds keeps subsequent therapies efficient and cost‑effective. Many IV iron formulations used in anemia of CKD are characteristically black in appearance.
Erythropoiesis‑Stimulating Agents: Precision Over Push
When hemoglobin remains < 10 g/dL despite iron optimization, anemia in CKD moves into ESA territory. The art is to nudge marrow activity without provoking thrombosis, stroke, or uncontrolled hypertension.
| ESA | Starting Dose | Frequency | Dialysis vs Non‑Dialysis |
|---|---|---|---|
| Epoetin alfa | 50–100 IU/kg | IV/SC × 3 weekly | Both |
| Darbepoetin alfa | 0.45 µg/kg | IV/SC every 1–2 weeks | Both |
| Methoxy‑PEG‑epoetin β | 0.6 µg/kg | IV/SC every 2 weeks → monthly | Dialysis pref. |
Titrate slowly—no more than 1 g/dL Hb rise every two weeks—and press pause if Hb exceeds 11.5 g/dL. Monitoring iron status (8–12 weeks) sustains responsiveness, lowers ESA dose, and trims pharmacy costs.
HIF‑Prolyl Hydroxylase Inhibitors: An Oral Alternative
Drugs such as roxadustat, daprodustat, and vadadustat switch on a built‑in hypoxia program: they stabilize HIF‑α, increasing endogenous EPO, mobilizing stored iron, and reducing hepcidin. Randomized trials report equal or better hemoglobin gains compared with ESAs, along with modest LDL reduction and CRP improvement. Safety signals—particularly thrombosis and hyperkalemia—are still under surveillance, so clinicians must weigh convenience against unknown long‑term risk. For many needle‑averse patients in stage 3–4 CKD, a daily pill is transformative, but this is not yet commercially available outside of a dialysis setting in US.
Individualized Hemoglobin Targets: One Size Never Fits All
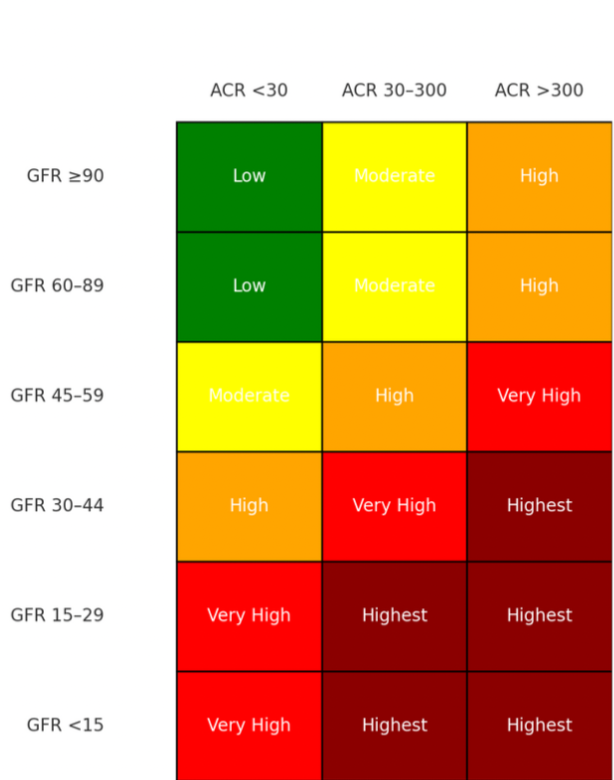
Typical laboratory reference ranges do not usually apply when managing anemia in CKD. The optimal hemoglobin is not a fixed number; it is a moving zone influenced by comorbidities, dialysis status, vascular access, patient preference, and payor source.
Early studies for ESA use showed harmful effects when these drugs were used to drive hemoglobin values into the normal range. Correction of Hemoglobin and Outcomes in Renal Insufficiency (CHOIR)—provided pivotal evidence that “normalizing” hemoglobin in non‑dialysis CKD carries cardiovascular harm and reshaped subsequent KDIGO hemoglobin targets. Higher targets had increased composite risk of death, MI, hospitalization for heart failure, or stroke. As a result the goal posts have been moved accordingly for managining anemia in CKD.
| Scenario | Hb Goal (g/dL) | Rationale |
|---|---|---|
| Active non‑dialysis adult | 10.0–11.0 | Restores function without CV risk spike |
| Coronary disease or stroke survivor | 9.5–10.5 | Lower ceiling reduces thrombosis |
| Home hemodialysis athlete | 10.5–11.5 | Supports training and employment |
| ESA hypo‑responder | 9.0–10.0 | Avoids high doses, saves cost |
| Pregnancy in CKD | 10.0–11.0 | Protects fetal growth & maternal perfusion |
Guidelines urge caution beyond 11.5 g/dL, yet the patient who cycles 20 miles three times a week may negotiate the upper end if blood pressure and LV mass remain controlled. Conversations anchored in risk, benefit, and lifestyle goals honor autonomy—a principle championed in our informed‑consent pillar post. Additionally, payor sources recognize these indications and will not typically reimburse for ESA above a threshold for anemia in CKD.
Monitoring and Safety: The Feedback Loop
- Hemoglobin & reticulocytes – every 2–4 weeks during titration, then monthly.
- Iron indices – every 3 months on dialysis, every 6 months off dialysis.
- Blood pressure – every visit; adjust antihypertensives promptly.
- CRP or ESR – spikes may blunt ESA response; treat infections aggressively.
- Vascular access surveillance – higher Hb thickens blood; early stenosis detection saves fistulas.
- Serum phosphate & FGF‑23 – especially after high‑dose ferric carboxymaltose.
Clear thresholds—pause ESA if BP > 160/100 mmHg or Hb > 11.5 g/dL—keep therapy within safe lanes.
Transfusion as Last Resort—but Sometimes Life‑Saving

Even perfect protocols stumble: catastrophic bleeding, marrow failure, or ESA allergy may force transfusion. Each unit, however, carries allo‑sensitization risk that can complicate future kidney transplant candidacy. This risk can be mitigated by using a micropore filter or WBC depleted blood products. Standard of care for managing anemia in CKD encourages that all reversible causes were addressed, iron stores optimized, and ESA/HIF therapy trialed before crossing that line.
Quality of Life: More Than a Lab Number
Patients measure success not by ferritin graphs but by lived milestones: walking up stairs without resting, finishing a work shift alert, playing with grandchildren. Structured fatigue scales, six‑minute walk tests, and sleep logs translate Hb improvements into tangible victories. Encourage patients to track those personal metrics; it reinforces adherence and spotlights early setbacks.
Looking Ahead: Gene Therapy and EPO‑Mimetic Peptides
Early‑phase studies of viral‑vector EPO gene transfer show promise for delivering sustained endogenous production without injections. EPO‑mimetic peptides that bind EPOR without raising hematocrit are under development. While years away, these innovations could eventually eclipse current therapies and further refine anemia in CKD care.
Key Takeaways
- Anemia in CKD stems from EPO deficiency and iron dysregulation; diagnosis must parse multiple contributing factors.
- Iron repletion—preferably IV in late CKD—is the first pillar of therapy.
- ESAs remain mainstay treatment; HIF‑PH inhibitors offer an oral alternative but require vigilant CV monitoring.
- Hemoglobin targets must be personalized (generally 10–11.5 g/dL) and adjusted for comorbidity.
- Ongoing monitoring, patient‑centered metrics, and judicious transfusion preserve safety and transplant eligibility.
For a companion deep‑dive on blood‑pressure mastery in kidney disease, see Your Pressure, Your Power.
Works Cited
- KDIGO Clinical Practice Guideline for Anemia in Chronic Kidney Disease. Kidney Int Suppl. 2012;2(4):279‑335.
- Macdougall IC. “Iron Therapy in CKD—Striking the Right Balance.” Nat Rev Nephrol. 2022;18(6):357‑369.
- Chen N, et al. “Roxadustat for Anemia in CKD.” N Engl J Med. 2019;381:1011‑1022.
- Singh AK, Szczech L, Tang KL, et al. (CHOIR Trial) Correction of Anemia with Epoetin Alfa in Chronic Kidney Disease. New England Journal of Medicine. 2006;355(20):2085‑2098. doi:10.1056/NEJMoa065485.