Most CKD Patients Die of Heart Disease — Not Kidney Failure
Protecting your kidneys also means protecting your heart.
Here’s how chronic kidney disease (CKD) silently increases your risk of heart disease — and what you can do to protect both.
Two Organs, One Fate: The Heart-Kidney Connection in CKD
When people hear “chronic kidney disease,” they often imagine dialysis machines or transplant lists. But here’s the clinical truth that surprises many: most people with CKD don’t die because their kidneys fail — they die from heart disease.
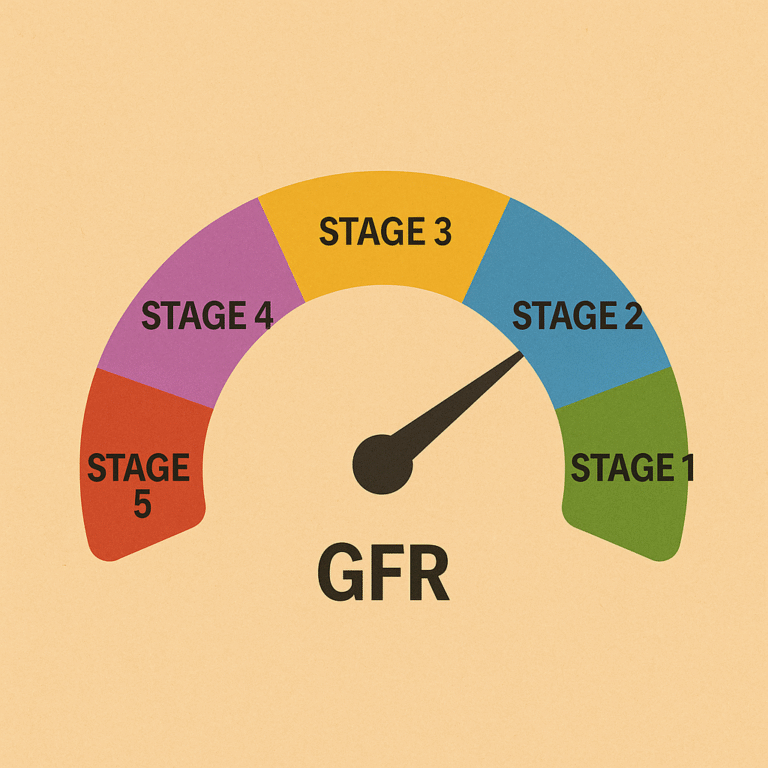
That isn’t fearmongering. It’s a fact supported by decades of research and reinforced by what physicians observe in practice every day. Even in the early stages of CKD, the risk of heart disease — including heart attacks, strokes, arrhythmias, and heart failure — begins to climb. By stage 3, the cardiovascular threat becomes as serious as that seen in diabetes.
Understanding this connection is critical. The heart and kidneys don’t operate in isolation. They’re biologically linked in ways that make damage to one organ a risk to the other.
The Heart-Kidney Connection: More Than Circulation
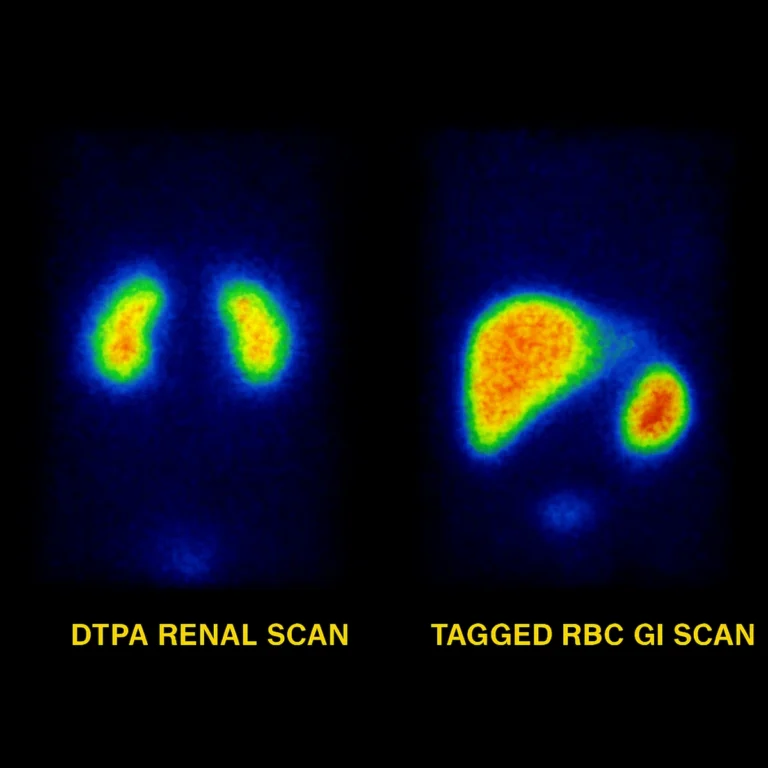
At first glance, the relationship between your heart and kidneys seems mechanical — the heart pumps blood, and the kidneys filter it. But the connection is more intricate than simple plumbing.
The kidneys are deeply involved in regulating key processes that impact heart health:
- Blood pressure control, which affects how hard the heart must work
- Electrolyte balance, especially potassium and calcium, which influence heart rhythm
- Red blood cell production, via erythropoietin, which affects oxygen delivery to the heart
- Fluid volume regulation, determining whether the heart faces a normal load or excess strain
As kidney function declines, these systems begin to falter — quietly, systemically, and with real consequences for the heart. That’s why heart disease is not just a side concern in CKD — it’s often the main threat.
Why CKD Raises the Risk of Heart Disease
CKD is a powerful risk multiplier. It doesn’t simply add risk for heart disease — it compounds it, creating the ideal environment for vascular damage, inflammation, and heart strain.
1. Hypertension
Damaged kidneys retain more sodium and water, raising blood pressure. Chronic hypertension stiffens arteries, enlarges the heart, and accelerates the formation of plaque — all of which feed into heart disease.
2. Anemia
Reduced erythropoietin leads to fewer red blood cells. The heart compensates by pumping harder, which over time can cause thickening of the heart wall (left ventricular hypertrophy) and reduced efficiency.
3. Vascular Calcification
Disrupted calcium and phosphorus levels in CKD lead to calcification of arteries and heart valves. This makes them stiff and less responsive, increasing the risk of heart disease and valvular dysfunction.
4. Uremic Toxins
As waste products build up in CKD, they promote inflammation, oxidative stress, and endothelial damage — all major drivers of atherosclerosis and cardiovascular disease.
5. Shared Risk Factors
CKD rarely occurs alone. It often exists alongside diabetes, obesity, and dyslipidemia — each of which increases the risk of heart disease. Together, these conditions amplify the danger.
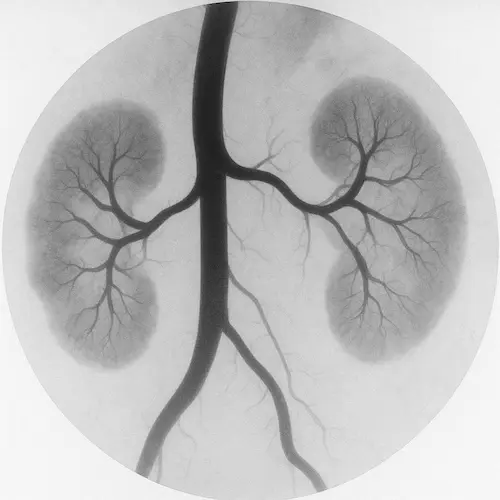
Why the Heart Drives the Kidneys
The kidneys are highly flow-dependent organs, relying on robust cardiac output to receive adequate blood supply — in fact, they receive up to 30% of each heartbeat’s output. This intimate reliance on circulation helps explain why high blood pressure is so damaging to kidney function over time: it not only injures the delicate filtering units but also signals broader vascular strain. In cases of chronic heart failure, kidney function often declines in parallel — not because the kidneys are directly diseased, but because they become innocent bystanders to falling cardiac performance.
This interdependence doesn’t end with disease progression — it also influences treatment. For example, conventional hemodialysis requires sufficient cardiac strength to tolerate the shifting fluid and to maintain forward flow into the machine. While the dialysis circuit includes a pump to return blood, it’s still the patient’s heart that must supply it in the first place. Without adequate cardiac support, dialysis becomes not just harder — but sometimes, untenable.

The Numbers Don’t Lie
According to the National Kidney Foundation:
- Adults with stage 3 CKD are twice as likely to die from heart disease as from kidney failure.
- In stage 4 and 5, that cardiovascular risk triples or more.
- Even mild proteinuria (microalbuminuria) — with normal filtration rates — is linked to increased heart attack and stroke risk.
Because of this, CKD is now officially recognized in many clinical guidelines as a “coronary heart disease risk equivalent.” That means having CKD should trigger the same level of preventive care and vigilance as having known heart disease.
How to Protect Both Organs
The encouraging news? Many of the strategies that help your kidneys also help prevent heart disease.
Key Actions to Reduce Heart Disease Risk in CKD:
- Control blood pressure to below 130/80 mmHg, often using ACE inhibitors or ARBs
- Manage blood sugar if diabetic, aiming for A1C <7% or as advised
- Lower cholesterol with statins or other agents when appropriate
- Avoid tobacco, which accelerates vascular damage
- Exercise regularly, with clearance from your doctor
- Eat a kidney- and heart-friendly diet, low in sodium, phosphate additives, and ultra-processed foods
These interventions not only protect the kidneys but are proven to reduce the risk of heart disease and extend lifespan.
Watch Your Labs, Watch Your Heart
Keeping tabs on potassium, phosphorus, calcium, and PTH is vital. Shifts in these labs often happen before symptoms appear, and imbalances can directly increase your risk of heart disease.
Ask your provider to explain trends over time — not just isolated values. Advocate for action when things are drifting out of range.
The Role of Coordinated Care
One of the most overlooked dangers in CKD is fragmented care. You may see multiple specialists, but unless those teams are communicating, no one may be looking at the full picture.
Make sure your cardiologist and nephrologist share notes — or help them do so.
Consider adding:
- A renal dietitian to guide your food choices
- A clinical pharmacist to help manage complex meds
- A heart failure specialist if symptoms like fatigue or swelling occur
You are the common thread — and understanding how heart disease and CKD are connected can empower you to speak up and shape your care.
The Takeaway
Chronic kidney disease is more than a kidney issue — it’s a direct threat to your heart.
Left unaddressed, CKD silently increases your risk of heart disease, often before you feel a single symptom. But with the right strategy, you can protect both organs — and extend both quality and quantity of life.
Don’t wait for chest pain to start thinking about your heart.
If you’re managing CKD, you’re already at risk for heart disease — whether you realize it or not.
References
Gansevoort RT, et al. Chronic kidney disease and cardiovascular risk: Epidemiology, mechanisms, and prevention. Lancet. 2013;382(9889):339–352.
KDIGO 2021 Clinical Practice Guidelines for Cardiovascular Disease in CKD. Kidney Int Suppl. 2021;11(3):S1–S59.
National Kidney Foundation. Heart disease and CKD. https://www.kidney.org/atoz/content/heart-disease