Choosing the Right Path for Your Quality of Life: 4 Dialysis Modality Options
When kidneys fail, life continues—but it changes. You may feel that your body has betrayed you, or that your options are narrowing. But in reality, the decision to begin dialysis opens the door to multiple possible paths, each shaped by how you live, what you value, and the support systems around you.
Choosing a dialysis modality isn’t just a medical decision—it’s a life decision. Some patients prefer the security of a clinic. Others crave independence and control. And for some, the best path is one that doesn’t include dialysis at all. The right choice depends not just on your kidney function, but on your vision for how you want to spend your time, preserve your energy, and maintain your dignity.
In this article, we explore the four primary options available when kidney function declines beyond the point of recovery:
- In-center hemodialysis
- Home hemodialysis
- Peritoneal dialysis
- Conservative management (non-dialytic therapy)
Each dialysis modality brings its own set of routines, responsibilities, and tradeoffs. By understanding them clearly, you can choose the one that best fits your quality of life—and revisit that decision as your needs evolve.
Why Modality Matters: Treatment Should Fit the Person, Not the Other Way Around
Too often, dialysis is introduced in a moment of crisis. A patient becomes suddenly ill, lands in the hospital, and is told it’s time to “start treatment.” But what kind of treatment? On what terms? With what vision of life after that first session?
Dialysis isn’t just a machine—it’s a structure. It changes your weeks, your sleep, your diet, your travel. That’s why the dialysis modality you choose matters so much. It shapes not only your medical outcomes but your daily rhythm and sense of control.
When patients are given time, education, and choice, they report higher satisfaction with their care. They also tend to start treatment in safer ways, with planned access rather than emergency catheters, and with greater readiness for the journey ahead.
Knowing your dialysis modality options early can change everything.
In-Center Hemodialysis: Structure and Supervision in a Clinical Setting

In-center hemodialysis is the most familiar form of kidney replacement therapy. Patients typically go to a dialysis clinic three times per week, where nurses and technicians manage all aspects of treatment. Each session lasts about four hours, during which the patient’s blood is circulated through a dialyzer, filtered, and returned to the body.
For many, this dialysis modality offers a sense of routine. The environment is predictable. Clinical staff are always available. Vitals are monitored continuously. Some patients enjoy the social interactions—seeing the same faces, sharing a quiet camaraderie with others on the same path.
But structure can also feel like rigidity. The fixed schedule may interfere with work or family events. Transportation becomes a recurring burden, especially for those with mobility limitations or rural addresses. And the intensity of fluid and toxin shifts during treatment can leave patients feeling exhausted afterward.
Still, for patients who prefer not to self-manage, or who feel comforted by professional oversight, this dialysis modality remains a safe and reliable choice. It’s especially suitable for those who live alone, have cognitive impairment, or face barriers to setting up care at home.
Home Hemodialysis: Flexibility Through Independence

Home hemodialysis allows patients to perform their own treatments in the comfort of their home. With adequate training and support, patients can use portable machines to dialyze on a schedule that works for them—sometimes shorter and more frequent sessions during the day, or longer treatments overnight while they sleep.
This dialysis modality offers powerful benefits. Because treatments can be done more often, fluid and waste removal is gentler and more physiologically natural. Many patients report improved appetite, energy, and blood pressure control. The freedom to schedule sessions around work or family obligations can make a profound difference in lifestyle.
But home hemodialysis also requires commitment. Training takes several weeks, and patients must learn to operate machines, insert needles, monitor for complications, and respond to alarms. Most programs require a care partner to be present during treatment, though solo protocols exist in select settings.
There’s also a psychological shift involved. Taking responsibility for your own life-sustaining therapy can be empowering—but also anxiety-provoking. Some patients embrace it. Others feel overwhelmed.
When successful, though, this dialysis modality can restore a sense of agency and dramatically improve quality of life. It suits those who are confident, motivated, and supported—people who want to bring their care home on their own terms.
Peritoneal Dialysis: A Gentle, Internal Approach to Kidney Support
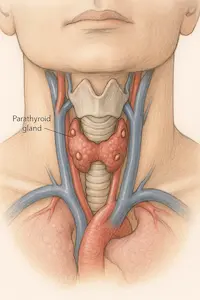
Peritoneal dialysis works differently. Instead of filtering blood through an external machine, this method uses the natural lining of your abdominal cavity—the peritoneum—as a dialysis membrane. A soft catheter is surgically placed into your abdomen, through which sterile fluid is exchanged several times per day.

There are two main ways to perform this dialysis modality:
- Continuous Ambulatory Peritoneal Dialysis (CAPD): Manual exchanges done during waking hours, each taking about 30 minutes.
- Automated Peritoneal Dialysis (APD): Performed overnight with a small machine (cycler), allowing patients to sleep while dialysis occurs.
Peritoneal dialysis is often praised for its gentleness. Because fluid removal happens gradually, there’s less risk of sudden blood pressure drops or cramping. Many patients feel more stable throughout the day. There are no needles, and no regular trips to a center are required. Patients often continue to work, travel, or attend school with minimal disruption.
But this dialysis modality requires discipline. Sterile technique is essential to prevent peritonitis, a serious abdominal infection. The catheter must be kept clean and secure. Some patients struggle with body image concerns or find the idea of a permanent abdominal access unsettling.
Still, for those who prefer to avoid needles and value freedom, PD can offer unmatched lifestyle advantages. It often suits people with intact cognitive function, stable living conditions, and a strong desire for independence.
Conservative Management: Support Without Dialysis

For some patients, the best choice may be to forgo dialysis entirely. This is not about giving up—it’s about making a values-based decision to prioritize comfort, clarity, and time over medical intervention.
Conservative, non-dialytic management is a medically supported alternative to choosing a dialysis modality. This path is intended for patients who either do not want dialysis or are unlikely to benefit meaningfully from it. It is often appropriate for older adults with multiple chronic conditions or advanced frailty.
Instead of starting dialysis, these patients receive careful medical management of symptoms:
- Medications to control fluid overload, nausea, or itching
- Adjustments to diet and medications for blood pressure, potassium, or phosphorus
- Emotional and palliative care support to preserve quality of life
This approach requires honesty, trust, and communication. Patients should be counseled early—ideally during Stage 4 CKD—so that they understand what to expect and can prepare with dignity. Families should be involved, and transitions to hospice care should be proactive, not reactive.
Choosing conservative care is not choosing death. It’s choosing a life defined by peace and intention, supported by a care team that honors the human experience as much as the lab values.
Making the Choice: What Really Matters in a Dialysis Modality
Selecting a dialysis modality is never just a clinical decision. It’s a deeply personal one. You are not just choosing a machine—you’re choosing how to spend your mornings, how to travel, whether you’ll need a caregiver nearby, what kind of risks you’re willing to tolerate, and how much control you want over your care.
So what matters most?
- Your lifestyle: Do you want flexibility? Routine? Privacy?
- Your home environment: Do you have space, support, stability?
- Your health status: Are you able to insert needles, manage machines, or follow sterile technique?
- Your emotional needs: Do you find comfort in structure or in independence?
- Your goals: Are you aiming to extend time, minimize disruption, or preserve comfort?
This decision doesn’t need to be rushed—and it doesn’t need to be permanent. Many patients transition from one dialysis modality to another as their needs and circumstances change. What matters is that the dialysis modality you choose supports who you are and what you value.
The Role of Education: Time Makes the Difference
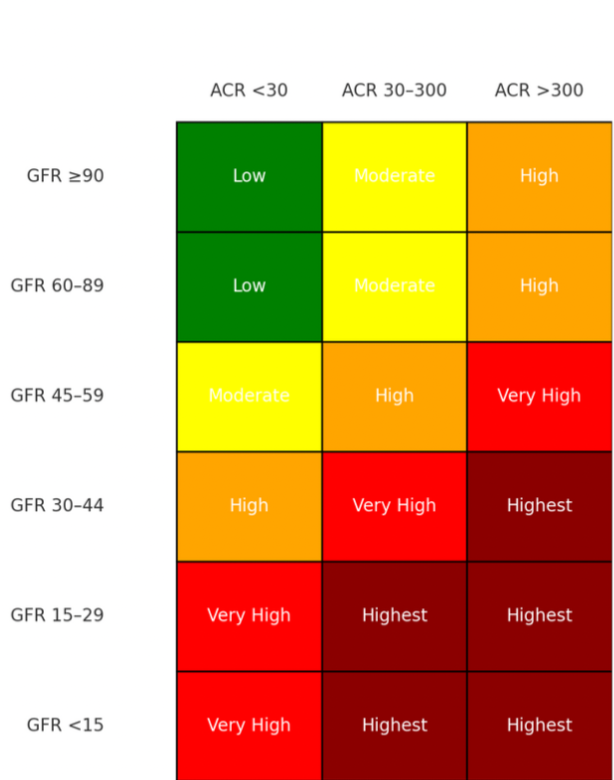
The best outcomes occur when patients are given time to make an informed decision. Education should begin during the early stages of kidney disease, ideally before eGFR drops below 20 mL/min. At this stage, you can still plan your access, coordinate support systems, and prepare emotionally.
Ask your nephrology team for:
- A referral to a modality education class
- Written and video materials explaining each dialysis modality
- Opportunities to meet other patients who have lived these choices
- A social worker or care navigator to help you assess home readiness
Education is not persuasion. It’s empowerment. And it can mean the difference between starting dialysis in fear and starting it with confidence.
Preemptive Transplant: A Fifth Path for Eligible Patients
While most discussions focus on dialysis and conservative care, some patients may qualify for a preemptive kidney transplant—a transplant performed before dialysis ever begins. This option is generally available to individuals who have a medically suitable living donor candidate, such as a family member or close friend. Preemptive transplantation is associated with better long-term outcomes, including improved survival and quality of life compared to starting on dialysis first. It requires early referral to a transplant center, thorough evaluation of both donor and recipient, and careful timing. For patients facing kidney failure with a supportive donor in place, this fifth option offers the possibility of avoiding dialysis entirely.
???? Works Cited
- KDIGO. “2020 Clinical Practice Guideline for the Management of Non-Dialysis CKD.” Kidney Int Suppl. 2020;10(4):S1–S135. https://kdigo.org
- Mehrotra R, Devuyst O, Davies SJ, Johnson DW. “The Current State of Peritoneal Dialysis.” J Am Soc Nephrol. 2016;27(11):3238–3252.
- Wong SPY, Kreuter W, O’Hare AM. “Treatment Intensity at the End of Life in Older Adults Receiving Long-term Dialysis.” Arch Intern Med. 2012;172(8):661–663.
- National Kidney Foundation. “Choosing a Treatment for Kidney Failure.” https://www.kidney.org/atoz/content/dialysisinfo