Hemodialysis Adequacy – Understanding this Important Value
The transition from chronic kidney disease to thrice-weekly blood purification is daunting, but knowing the science behind each session turns anxiety into agency. At the center of that science is hemodialysis adequacy—the quantitative snapshot of how completely a treatment eliminates uremic toxins and extra fluid.
Think of it as the report card that determines whether your body can cruise smoothly until the next appointment. When hemodialysis adequacy is on point you wake with clearer thinking, steadier appetite, and less restless-leg irritation at night. When it slips, fatigue and swelling often creep in before lab numbers sound the alarm. By unpacking the methods, the measurements, and the modifiable levers that influence hemodialysis adequacy, you equip yourself to play an active role in preserving health and quality of life.
What Is Hemodialysis Adequacy?
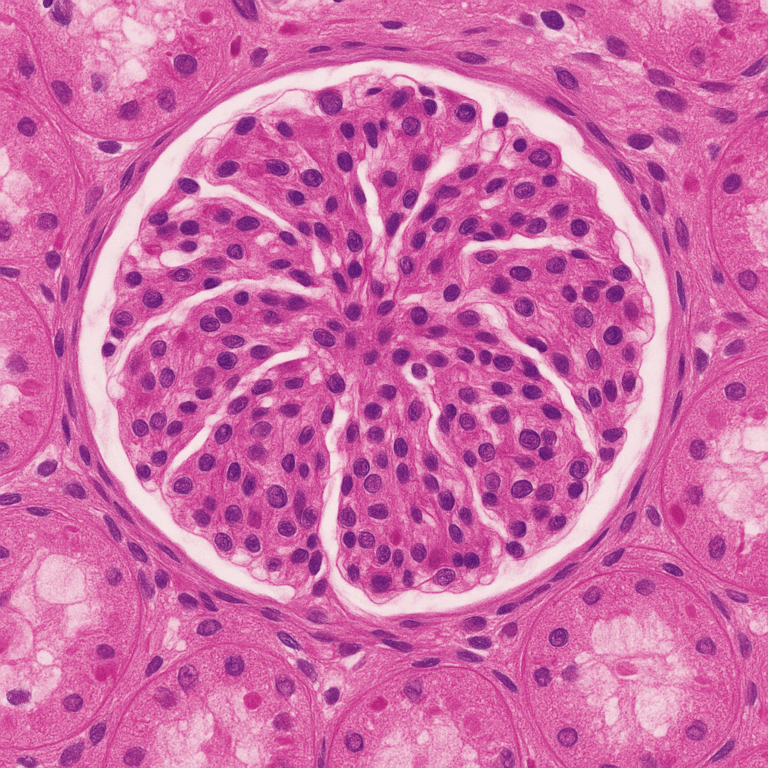
Every dialysis machine hums with the same goal: to replicate enough kidney function to keep you safe between treatments. Clinicians gauge success using several formulas, but the workhorse is Kt/V. In this equation K represents the dialyzer’s clearance rate, t is session length, and V is the volume of water inside your body. For people on a conventional Monday-Wednesday-Friday or Tuesday-Thursday-Saturday schedule, a single-pool Kt/V of ≥ 1.20 is the accepted threshold of acceptable hemodialysis adequacy. When computed across the entire week, that number should translate into removing roughly the same total urea a healthy pair of kidneys would excrete each day.
Numbers, however, cannot capture lived experience in isolation. Ask longtime patients what adequacy means and you will hear stories of sharper mental focus, better appetite, and energy to babysit grandchildren after an afternoon run. Adequate dialysis lowers hospitalization rates, curbs phosphorus levels that weaken bones, and supports cardiovascular resilience by preventing chronic fluid overload. In other words, hemodialysis adequacy is both a laboratory target and an everyday feeling of wellness.
Precision matters. A fistula with sluggish flow, a shortened session, or an unplanned weight gain can drag Kt/V downward by ten percent or more. Because urea rebounds into the bloodstream after the machine stops, even small deviations accumulate over time. Most dialysis units therefore run monthly labs and review clearance numbers chair-side: if hemodialysis adequacy falls below target twice in a row, the team investigates immediately rather than waiting for symptoms to bloom.
Why Adequacy Matters to Everyday Well-Being
The clinical literature links strong hemodialysis adequacy with fewer emergency-room visits, lower heart-failure rates, and better survival. Yet the benefit patients notice first is the return of vigor. When sufficient urea and phosphate are cleared, red blood cells carry oxygen more efficiently, nerves fire with less irritation, and muscles cramp less during sleep. Blood pressure stabilizes because the heart no longer wrestles with excess fluid, and phosphorus-driven bone pain eases when mineral balance is restored.
Adequacy also shapes long-term goals: preserving residual kidney function, keeping parathyroid hormone in check, and protecting vascular access. Each of these goals improves transplant candidacy and opens doors to home therapies that offer greater independence. Falling short of hemodialysis adequacy targets, on the other hand, elevates the risk of dialysis-related amyloidosis, accelerates coronary calcification, and magnifies the burden of anemia. In short, adequacy is not paperwork—it is the scaffolding on which a fulfilling life with dialysis is built.
How Adequacy Is Measured: From Kt/V to URR and Beyond
Although Kt/V dominates adequacy conversations, your monthly lab sheet likely lists a companion metric: the Urea Reduction Ratio (URR). URR calculates the percentage drop in blood-urea nitrogen from the start to the end of treatment; a value of ≥ 65 % usually corresponds to satisfactory hemodialysis adequacy. High-flux dialyzer programs or online hemodiafiltration may track β-2 microglobulin to confirm middle-molecule clearance.

Equilibrated Kt/V (eKt/V) refines the classic formula by accounting for post-dialysis rebound. While spKt/V ≥ 1.20 is the minimum, eKt/V aims for ≥ 1.05, highlighting the value of longer—or more frequent—sessions. Modern machines upload clearance data to cloud portals, letting you and your care team spot trends between monthly blood draws. Seeing hemodialysis adequacy plotted in real time transforms abstract math into a familiar health dashboard: when the line dips, interventions follow quickly.
Precise measurement is only half the task; correct sampling is equally vital. Drawing the post-dialysis blood sample at least two minutes after treatment stops avoids “artificially” high values that can mask inadequate clearance. Staff must also ensure needles sit at least two inches apart in the fistula to prevent recirculation—a silent thief that can trim Kt/V by up to 20 % without triggering an alarm.
Important Note on Nutrition and Your Adequacy Numbers
If you’re not eating enough protein, your pre-dialysis blood urea nitrogen (BUN) level can run low. That makes the percent-change calculations (URR and the Kt/V formula) look “good” even when only a small amount of waste is actually being removed. In other words, the numbers may tell one story while your body tells another—fatigue, weight loss, or a drop in appetite.
If pre-BUN keeps drifting downward, ask your dietitian to review your protein intake (most people on hemodialysis need at least 1–1.2 g of protein per kilogram each day) and have your care team check other nutrition markers like albumin and unintentional weight change. Healthy eating keeps the lab values honest and ensures your dialysis prescription truly meets your needs.
Modifiable Drivers of Hemodialysis Adequacy
Enhancing hemodialysis adequacy often starts with small prescription tweaks: raising blood-flow rate from 350 to 400 mL/min, swapping a 1.8 m² dialyzer for a 2.0 m² membrane, or extending each session by fifteen minutes. Increasing dialysate flow (Qd) from 600 to 800 mL/min yields an immediate jump in urea clearance, especially with high-flux filters. Frequency matters too; adding a fourth weekly run or switching to short-daily home treatments can push weekly Kt/V past 2.0, mirroring native-kidney toxin removal.
Prescription, however, is just half of the equation. A healthy fistula or graft keeps blood moving smoothly through the circuit. Daily palpation for thrill and monthly ultrasound surveillance detect stenosis early, protecting the access that underpins every measure of hemodialysis adequacy. Fluid management matters: arriving for treatment at or near your prescribed dry weight prevents aggressive ultrafiltration that can shorten session time or leave you dizzy and hypotensive.
Lifestyle choices strengthen clinical strategies. Moderate intradialytic cycling may enhance solute removal by boosting muscle perfusion, while a dietitian-guided plan that limits phosphorus additives reduces the toxin load facing each session. Consistency is key: missing even one treatment can reduce average weekly adequacy by 15 %, undoing weeks of meticulous attention.
Modifiable Factors
- Blood-flow rate
- Dialysate flow rate
- Dialyzer membrane properties
- Treatment time
- Needle placement
- Access flow
- Timing of blood draw
- Arriving near target weight
These items either raise or preserve the dialyzer’s clearance (K), extend t (time on the machine), or influence body-water volume V—making them the key levers for optimizing Kt/V and, by extension, overall hemodialysis adequacy.
Home Hemodialysis Adequacy: Modified Targets
Because home programs deliver treatments more frequently—often five to six days per week, sometimes overnight—hemodialysis adequacy is calculated across the entire week rather than per session. The benchmark many programs use is a weekly standard Kt/V ≥ 2.0, which reflects the cumulative clearance from several gentler runs.
Frequent, longer, or nocturnal sessions spread the work over more hours, lowering the “dose” each treatment must deliver while better mimicking continuous native-kidney filtration. This softer, steadier schedule improves blood-pressure control and phosphorus removal, but it also means single-run Kt/V values look lower than the ≥ 1.2 target used for thrice-weekly in-center dialysis. Evaluating adequacy therefore focuses on weekly totals and symptom trends rather than individual-session numbers, ensuring the prescription remains aligned with both physiological needs and the patient’s daily routine.
Warning Signs That Adequacy Has Slipped
Uremic toxins accumulate insidiously, so early signals are subtle: lingering metallic taste, creeping ankle swelling, or relentless fatigue despite a normal hemoglobin. Rising predialysis BUN, stubbornly high phosphorus, or a drop in URR confirm that hemodialysis adequacy needs reassessment. Your team may order access imaging, recalibrate dry weight, or recommend nocturnal in-center sessions that double treatment length without adding chair days.
Partnering With Your Team for Lasting Adequacy
Success thrives on transparency. Bring a symptom journal to monthly meetings, note any curtailed treatments, and report vascular-access changes. Many centers now print clearance reports after every run; reviewing these numbers empowers you to see hemodialysis adequacy as a dynamic parameter you co-manage. When life events—travel, illness, surgery—threaten routine, proactive schedule adjustments avert dips in clearance and preserve momentum.

In the end, hemodialysis adequacy is not an abstract statistic but a compass guiding lifestyle, prescription, and partnership decisions that shape vitality. By understanding how Kt/V and URR translate into sharper cognition, stronger bones, and a healthier heart, you reclaim agency in your dialysis journey. Stay informed, stay engaged, and let adequacy targets illuminate the path toward confident kidney care.
Also read about Peritoneal Dialysis adequacy : Peritoneal Dialysis Adequacy – The Key to Determining the Most Efficient Prescription
References
- Kidney Disease Outcomes Quality Initiative (KDOQI). Clinical Practice Guideline for Hemodialysis Adequacy. National Kidney Foundation; 2015.
- Kim EJ, Paik J, Davenport A. “Optimizing Dialysis Dose in Contemporary Practice.” Seminars in Dialysis. 2024; 37(1):12-24.
- Kidney Disease: Improving Global Outcomes (KDIGO). Clinical Practice Guideline on Peritoneal Dialysis Adequacy. 2021.