High Blood Pressure and Kidney Disease: 5 Ways to Change for the Better.
High blood pressure and kidney disease are locked in a dangerous tug-of-war. This two-way relationship causes damage in both directions—and often goes unnoticed until the damage is done. Understanding this connection can help you break the cycle and protect your long-term kidney function.
How High Blood Pressure and Kidney Disease Damage Each Other
High blood pressure is one of the most common chronic conditions in the world. It’s called the “silent killer” because it rarely causes symptoms—yet over time, it can quietly damage your heart, brain, blood vessels… and kidneys.
In fact, high blood pressure and kidney disease are deeply intertwined. High blood pressure is the second leading cause of chronic kidney disease (CKD) in the U.S., just behind diabetes. But the relationship goes both ways: as kidney function worsens, it can drive blood pressure even higher.
How High Blood Pressure Hurts the Kidneys
Your kidneys contain millions of tiny blood vessels (glomeruli) that filter your blood. When blood pressure is too high, it puts excessive force on these vessels. Over time, this causes:
- Thickened and narrowed vessels, reducing blood flow
- Scarring (nephrosclerosis), which impairs filtering ability
- Leakage of protein into the urine, a hallmark of kidney damage
- Gradual loss of kidney function, sometimes without symptoms
If left unchecked, high blood pressure and kidney disease can drive each other forward, leading to worsening CKD and eventually kidney failure.
When CKD Causes High Blood Pressure
The reverse is also true. As kidney function declines:
- Fluid builds up in the body
- The kidneys stop producing enough renin and other blood pressure–regulating hormones
- Salt and water retention become more pronounced
These changes can cause or worsen high blood pressure, creating a vicious cycle. That’s why treating high blood pressure and kidney disease together is essential.
As nephrologists often say: “You can’t treat CKD without managing the blood pressure.”
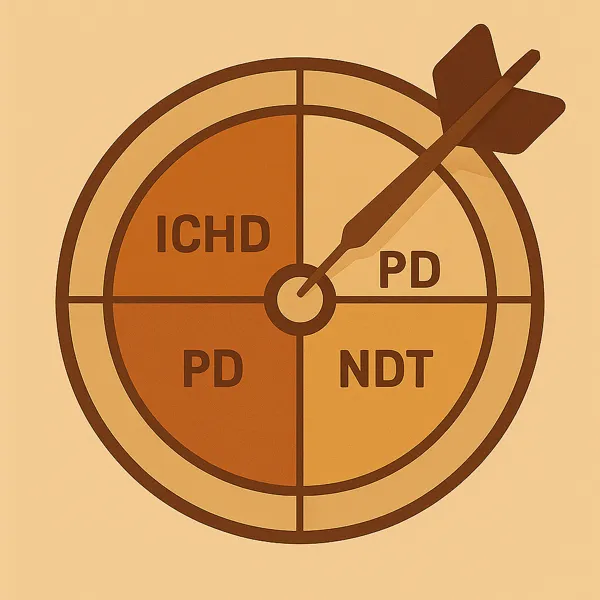
What Blood Pressure Is Too High?

For patients with high blood pressure and kidney disease, most guidelines recommend keeping readings below 130/80 mmHg. This target is tighter than for the general public but is supported by strong evidence showing it slows kidney decline.
However, blood pressure goals may be adjusted for older adults or those with other medical conditions. Always work with your care team to find the right range for you.
Taking Control: What You Can Do
The good news is that both high blood pressure and kidney disease are treatable—especially when caught early. Here’s how to take action:
1. Medication Matters
- First-line treatments include ACE inhibitors or ARBs (e.g., lisinopril, losartan)
- These medications not only lower blood pressure but also reduce protein leakage
- Multiple medications are often needed—and that’s okay
2. Cut the Salt
- Most Americans consume over 3,400 mg of sodium per day—well above the kidney-friendly limit of 2,300 mg
- Reducing sodium helps lower blood pressure and reduce fluid retention
3. Move More
- Even modest physical activity (e.g., 30-minute walks) can reduce blood pressure naturally
4. Manage Stress
- Chronic stress elevates blood pressure and undermines kidney function
- Mindfulness, breathing exercises, and better sleep all help

5. Stay Informed
- Monitor your blood pressure at home regularly
- Share readings with your care team
- Ask: “Is my target based on my kidneys or my age?”
The Takeaway
High blood pressure and kidney disease feed into each other—but they’re also among the most controllable risk factors in medicine.
If you’re at risk for CKD or already diagnosed, managing your blood pressure is one of the best things you can do to slow disease progression. Your efforts may not always show immediate results, but over time, they protect the very filters your life depends on.
Talk to your provider about a personalized blood pressure goal, get a reliable home monitor, and be consistent.
You won’t feel the damage happening—but with awareness and action, you can stop it.
Want to learn how patients can take charge of blood pressure in real life?
Read more in “Your Pressure, Your Power”
References
- Whelton PK, Carey RM, et al. 2017 ACC/AHA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure. Hypertension. 2018;71(6):e13–e115.
- Ku E, et al. Controlling hypertension in patients with CKD: A pathway to slowing progression. Adv Chronic Kidney Dis. 2015;22(2):116–123.
- National Kidney Foundation: High Blood Pressure & Your Kidneys – https://www.kidney.org/atoz/content/hbp