Imaging the Kidneys- 3 Important Options Include Ultrasound, CT and MRI
When it comes to understanding kidney health, lab tests like creatinine and eGFR often take center stage. That’s where imaging the kidneys becomes an essential part of both acute and chronic kidney care. Behind every lab result lies an organ with its own story—and sometimes, the only way to truly understand that story is by seeing it.
Whether you’re facing an unexpected episode of acute kidney injury (AKI) or managing chronic kidney disease (CKD) over time, imaging plays a quiet but critical role. It helps your doctors answer questions that lab results alone can’t resolve: Is there a blockage? Has the kidney structure changed? Is there evidence of long-term scarring—or something more urgent?
In this post, we’ll walk through the major tools used in nephrology for imaging the kidneys —ultrasound, CT scans, and MRI—to help you understand what each one offers, when it’s used, and how it fits into your kidney health journey.
Why Imaging the Kidneys Matters in AKI and CKD
Imaging the kidneys isn’t done on a whim. It’s a targeted way to gather visual evidence when something about kidney function—or kidney symptoms—raises concern. For patients with AKI, imaging helps rule out obstruction (like a kidney stone or enlarged prostate). In CKD, it helps confirm whether the damage is old and stable or if something new is evolving.
Doctors also use imaging to:
- Identify anatomical differences that might affect kidney function
- Detect cysts, tumors, or signs of inherited conditions (like polycystic kidney disease)
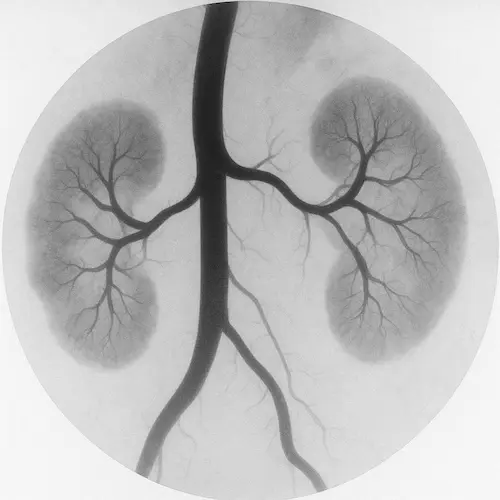
- Evaluate blood flow and vascular changes in advanced disease
- Confirm or question a diagnosis when lab values don’t tell the whole story
- Assess suitability and candidacy for diagnostic renal biopsy, if indicated.
Understanding what the kidneys look like often clarifies why they’re behaving the way they are.
Ultrasound: A Safe First Step in Kidney Imaging

Ultrasound is the workhorse of kidney imaging. It’s fast, painless, and doesn’t involve radiation or contrast dyes—making it ideal for first-line evaluation.
What can it show?
- Kidney size: Shrinking may indicate longstanding damage
- Echogenicity: Brightness on the screen suggests scarring or inflammation
- Obstruction: Hydronephrosis (swelling) can point to urine flow blockage
- Cysts and masses: Especially relevant in inherited or acquired cystic disease
Ultrasound is especially useful in:
- New AKI: Ruling out obstruction or hydronephrosis
- CKD progression: Determining if the kidneys are small and scarred
- Monitoring: Following known cysts or anatomical variants over time
Compared to other options for imaging the kidneys ultrasound has limits. It can’t visualize deeper tissue detail, and it’s less sensitive for detecting small stones or subtle vascular issues. Body habitus and operator skill can also affect image quality.
Still, for most patients, ultrasound remains the safest and most efficient way to begin imaging the kidneys.
CT Scans: A Closer Look at Structure and Obstruction
When ultrasound isn’t enough—or when something worrisome shows up—doctors may turn to CT scans for more detailed imaging.
A non-contrast CT is typically used when there’s concern for:
- Kidney stones: The gold standard for stone detection
- Obstruction: Assessing ureteral anatomy and flow issues
- Bleeding or trauma: Visualizing internal injury
A contrast-enhanced CT may be used for:
- Tumor detection or characterization
- Infection evaluation (such as an abscess)
- Pre-surgical planning
But there’s an important caveat: contrast agents used in CT imaging can be risky in patients with advanced CKD. While the risk of true contrast-induced nephropathy is now debated and likely overstated for many patients, caution is still warranted—especially if eGFR is under 30 mL/min/1.73m². In some cases, a non-contrast CT or alternative option for imaging the kidneys may be chosen instead.
CT also involves radiation exposure, which must be weighed carefully, especially in younger patients or those needing frequent imaging.
MRI and MRA: Specialized Tools for Vascular and Soft Tissue Insight
MRI (magnetic resonance imaging) offers exceptional soft-tissue resolution for imaging the kidneys without radiation. It’s often reserved for more complex or targeted questions, such as:
- Renal artery stenosis or vascular abnormalities
- Complex cysts or tumors requiring better soft tissue detail
- Patients who can’t tolerate contrast CT
MR angiography (MRA) provides a view of the kidney’s blood vessels without the need for iodinated contrast. Instead, gadolinium-based agents are used—but these come with their own risks in CKD.
In patients with eGFR under 30, gadolinium can very rarely trigger nephrogenic systemic fibrosis (NSF)—a serious and potentially disabling condition. The risk is extremely low with newer gadolinium agents and proper precautions, but it remains a consideration.
MRI is also slower and more expensive than other options, and it may not be readily available in all centers. However, for the right patient and the right question, MRI offers unparalleled detail—particularly when evaluating vascular disease or soft tissue masses.
Choosing the Right Test for the Right Patient
Selecting the right imaging study for imaging the kidneys isn’t about picking the most high-tech option. It’s about matching the imaging tool to the clinical need, considering:
- The question at hand (obstruction? mass? blood flow?)
- The patient’s kidney function and tolerance of contrast
- The urgency and diagnostic yield of the test
- Access, insurance, and local availability
In most cases:
- Ultrasound is first-line for unexplained AKI or stable CKD
- CT is second-line when detail or stone detection is needed
- MRI is used when vascular or soft-tissue evaluation is critical, or when CT contrast is contraindicated
Your provider considers these variables in real time—balancing diagnostic accuracy, patient safety, and resource availability.
What Imaging the Kidneys Can—and Can’t—Reveal
It’s important to know that imaging is a supportive tool, not a standalone diagnostic oracle. A normal ultrasound doesn’t mean kidney function is normal, and a CT scan may show stones without explaining why CKD is progressing.
Imaging:
- Can show structure, obstruction, scarring, size, asymmetry, masses
- Can’t directly show filtration rate, glomerular injury, or microscopic inflammation
That’s why imaging the kidneys is combined with lab work, urine studies, and your medical history to create a full picture of kidney health. Sometimes, even with extensive imaging, only a biopsy can give definitive answers about glomerular disease or early inflammatory damage.
Still, imaging provides something no blood test can: a visual record of what your kidneys have been through and what they’re facing now. When interpreted wisely, it helps shape a safer, more informed path forward.
???? Works Cited
- Levey AS, et al. “KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease.” Kidney Int Suppl. 2013;3(1):1–150. https://kdigo.org/guidelines/ckd-evaluation-and-management/
- Silver SA, et al. “Imaging and the Kidney: When, Why, and How.” Clin J Am Soc Nephrol. 2021;16(2):275–284.
- American College of Radiology. “Appropriateness Criteria®—Acute Renal Failure.” https://www.acr.org