When a Kidney Biopsy May Help — and 5 Important Things It Can Tell Us
When it comes to understanding kidney disease, few procedures provide as much insight as a kidney biopsy. Though often seen as a last resort, this test plays a central role in clarifying ambiguous lab results, identifying rare kidney conditions, and guiding treatment plans. But how do you know when it’s truly necessary—and what can it realistically reveal?
Let’s explore what prompts this decision, what to expect from the procedure, and how a tiny sample of tissue can shape your journey with chronic kidney disease (CKD) or other kidney disorders.
Not Every Case Needs a Biopsy
Most cases of chronic kidney disease can be diagnosed and managed without a biopsy. A careful combination of medical history, bloodwork, urinalysis, and imaging studies like kidney ultrasound can often tell the story. For example, diabetes, hypertension, or polycystic kidney disease usually leave characteristic footprints that are visible in lab patterns or imaging findings.
In these straightforward scenarios, adding an invasive procedure rarely changes the plan—and could introduce unnecessary risk.
When Suspicion Warrants Tissue
A kidney biopsy becomes necessary when the standard clues don’t quite fit. Imagine a patient with no history of diabetes or hypertension, yet their urine shows large amounts of protein, or their kidney function rapidly declines. Something is out of place. A biopsy offers the microscopic clarity needed to determine whether a condition like IgA nephropathy, lupus nephritis, vasculitis, or another glomerular disease is at work.
Key situations where a biopsy is typically considered include:
- Unexplained nephrotic-range proteinuria (typically >3.5 grams/day)
- Rapidly progressive glomerulonephritis (RPGN) with sudden loss of kidney function
- Hematuria with proteinuria and no clear cause
- Acute kidney injury (AKI) with unclear origin
- Suspected autoimmune disease affecting the kidneys, such as lupus
- Monitoring treatment response in known glomerular diseases
In transplant patients, biopsies are also used to evaluate rejection, drug toxicity, or recurrent disease.
What the Procedure Involves
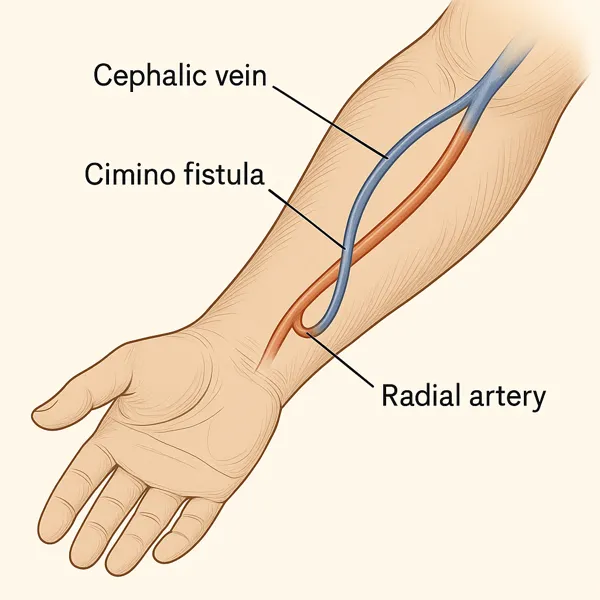
Despite sounding intimidating, a kidney biopsy is a relatively routine outpatient procedure. Using ultrasound (or occasionally CT) guidance, a nephrologist or interventional radiologist inserts a needle into the kidney to extract tiny samples of tissue. The patient is numbed beforehand, and conscious sedation may be used for comfort.
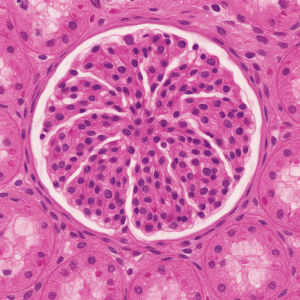
The collected tissue is then examined by a kidney pathologist using several types of staining and microscopy. In many cases, light microscopy, immunofluorescence, and electron microscopy are all used to assess for immune complex deposition, inflammation, scarring, and damage to specific kidney structures like the glomeruli or tubules.
The entire process—from needle stick to diagnosis—typically takes 1–3 days depending on lab complexity. The results provide a histologic diagnosis and may also be graded for severity and prognosis.
What a Biopsy Can (and Can’t) Tell You
A biopsy can:
- Confirm or rule out rare or overlapping diseases
- Determine if active inflammation is present (and whether it’s reversible)
- Guide treatment decisions, such as steroid or immunosuppressive therapy
- Assess whether a condition is mild or advanced
- Provide a clearer prognosis
However, it’s not a crystal ball. A biopsy can’t predict with certainty how fast your disease will progress, nor does it always lead to a curative treatment. In some chronic conditions, a biopsy simply confirms what’s already suspected without changing the therapeutic course. In others, it may reveal treatable inflammation and provide a powerful chance to intervene early.
Understanding the Risks
No medical procedure is without risk, and kidney biopsy is no exception. The most common complication is bleeding, which can occur around the kidney (perinephric hematoma) or in the urine (hematuria). Most cases are self-limited, but a small percentage may require hospitalization or intervention. Other rare risks include infection, injury to nearby structures, or very rarely, need for transfusion.
Your nephrologist will weigh these risks against the potential benefits. If the biopsy result is unlikely to change your management—or if the procedure itself poses undue risk—then it may be deferred in favor of close monitoring.
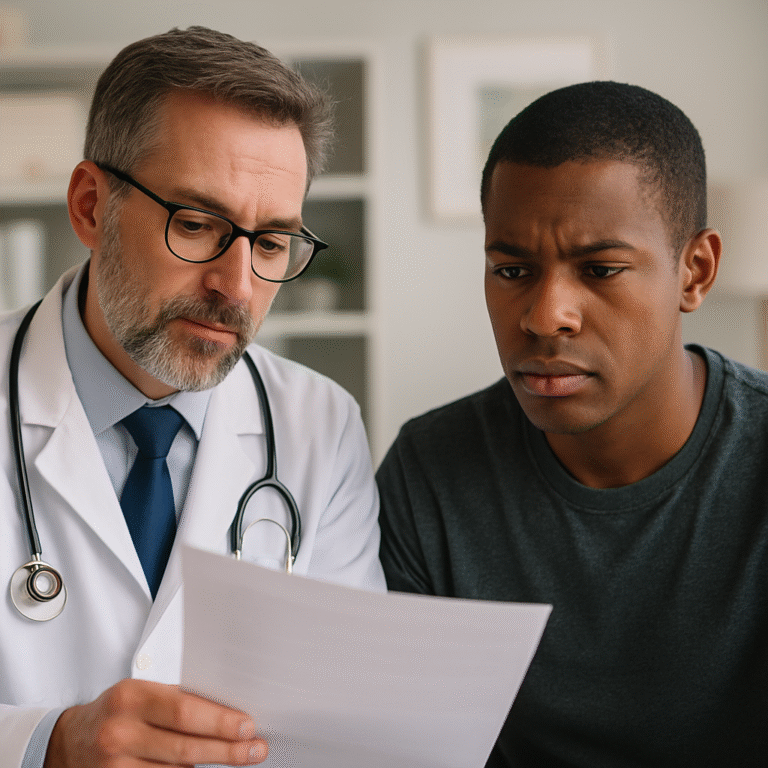
Making the Decision Together
The decision to undergo a kidney biopsy is rarely black-and-white. It often comes down to a nuanced conversation between patient and provider. If you’re facing that choice, ask:
- What are we trying to rule in or rule out?
- Will the result change how we treat this?
- Are there safer alternatives to consider first?
While a kidney biopsy can be a powerful diagnostic tool, the decision to proceed should never feel automatic. Informed consent means more than signing a form—it means having a thoughtful discussion between doctor and patient. The nephrologist must clearly explain why a biopsy is being considered, what information it may reveal, and how that information could affect treatment. They should also outline the risks, such as bleeding, infection, or the possibility of an inconclusive result, as well as any non-invasive alternatives that might exist.
Just as importantly, patients must be empowered to ask questions and weigh their own values and concerns. Some may choose to proceed immediately, while others may prefer to monitor and wait. Neither choice is wrong—because ultimately, the right decision is the one that aligns with the patient’s understanding, priorities, and comfort. Respecting autonomy is central to good kidney care.
Waiting for Results and Revised Plan of Care
Once the biopsy is complete and the tissue sample is analyzed, the waiting begins—often just a few days, but emotionally charged ones. The pathology report provides detailed insight into what’s happening at the microscopic level. Are there signs of inflammation, scarring, immune deposits, or structural abnormalities? These findings don’t just carry names—they carry implications. Some results may point toward conditions that are treatable with immunosuppressants, while others may reveal irreversible damage. Your nephrologist’s role is to walk you through these findings, translate the jargon into meaning, and help weigh the next steps. This is where biopsy becomes more than a procedure—it becomes a bridge between diagnosis and modification (or validation) of care plan.
Works Cited
- KDIGO Clinical Practice Guideline for Glomerulonephritis. Kidney Int Suppl. 2012;2(2):139–274.
- Fogo AB. Approach to renal biopsy. Am J Kidney Dis. 2003;42(4):826–836.
- Hogan J, Radhakrishnan J. The Spectrum of Minimal Change Disease in Adults. Clin J Am Soc Nephrol. 2013;8(3):475–483.
- Sethi S, D’Agati VD, Nast CC, et al. A proposal for standardized grading of chronic changes in native kidney biopsy specimens. Kidney Int. 2020;97(5):1052–1059.
Meta Description:
Curious about when a kidney biopsy is needed? Learn what this powerful diagnostic tool reveals—and when it’s worth the risk.