Groundbreaking Pig Kidney Transplants: A Breakthrough Path to Mainstream Renal Xenografts
The Promise of Pig Kidney Transplants.
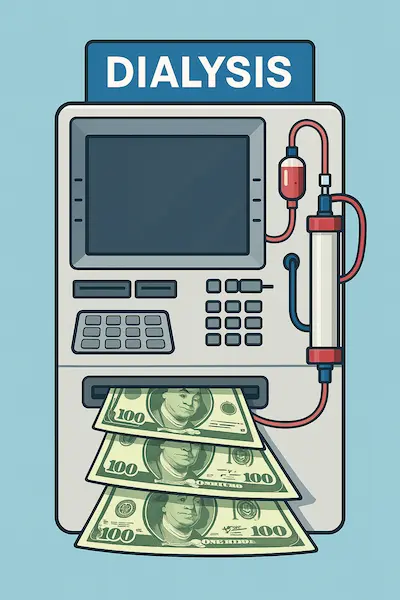
More than 100 000 Americans sit on the kidney-transplant wait-list today. A new option for transplantation is gaining traction. Pig transplant kidneys are a resurgent hot-topic and with all of the recent headlines, an evidence-based update is needed to separate fact from fiction. There is dire need for treatment options as the queue of patient’s seeking transplant grows by roughly a patient an hour. National Kidney Foundation Dialysis buys time, but cardiovascular risk, hospital days, and quality-of-life penalties remain harsh. A single viable alternative could change everything: the pig kidney transplant. What sounded like science fiction a decade ago is edging toward clinical reality as CRISPR-engineered porcine organs clear ever-higher safety and efficacy bars for human xenografts.
For patients and payers alike, the upside is enormous. A successful pig kidney transplant could:
- deliver immediate glomerular filtration without the ischemia time typical of deceased-donor grafts;
- slash dialysis expenditures (~US $90 000 per patient-year) and uninsured emergency visits;
- relieve the crushing psychosocial toll of indefinite “machine-life.”
Internal link: For background on the growing CKD burden, see our National Geographic wake-up call article.
How Renal Xenografts Work
- Biosecure donor herds. Pigs are reared in designated-pathogen-free (DPF) facilities, screened to eliminate porcine endogenous retroviruses (PERVs).
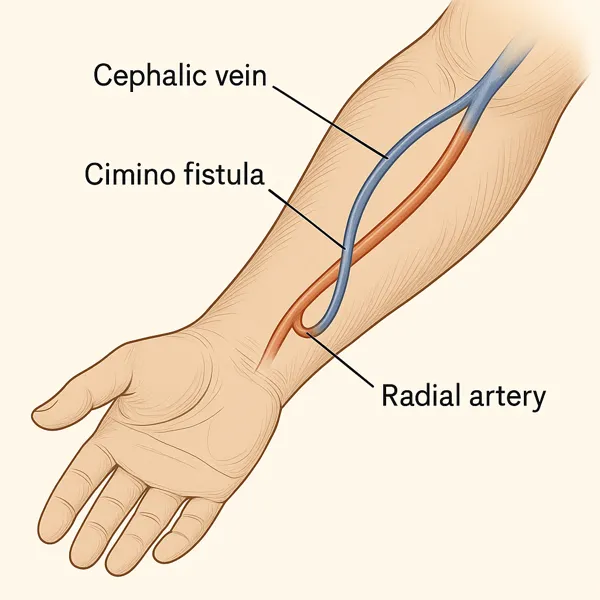
- CRISPR gene editing. Deletion of the α-Gal epitope and up-to-10 human “knock-ins” (e.g., CD46, thrombomodulin) blunt hyper-acute rejection and coagulation.
- Normothermic perfusion — Before implantation, the organ is flushed with oxygenated, hemoglobin-based solution to wash out residual porcine blood and prime endothelial metabolism.
- The operation. During the pig kidney transplant, surgeons anastomose the graft’s vessels and ureter to human counterparts; total clamp time now rivals routine living-donor surgery.
- Post-op management. Antibody-depleting induction plus costimulation-blockade (belatacept or anti-CD40) replaces calcineurin-heavy regimens, mitigating nephrotoxicity while targeting xenogeneic epitopes. KDIGO’s latest draft xenotransplant addendum echoes this approach.

Recent Breakthroughs & First-in-Human Trials
- 32-day sentinel model (NYU Langone, 2023). A gene-edited pig kidney transplant attached to a brain-dead donor produced urine and maintained creatinine for over a month, the longest functional xenograft on record at the time. NYU Langone Health
- First living recipient (Massachusetts General Hospital, March 2024). 62-year-old Rick Slayman left dialysis days after surgery; the graft functioned until his unrelated death eight weeks later, proving surgical and short-term safety. Massachusetts General Hospital (1)
- 130-day survival (NYU Langone, Nov 2024 – Apr 2025). Alabama patient Towana Looney showed stable eGFR before immune escape forced graft removal at day 130, yielding critical data on antibody-mediated rejection kinetics and informing trial immunosuppression design. AP News
- Regulatory green light (FDA, Feb 2025). Two biotech firms received IND approval to launch phase I “compassionate allotment” studies of pig kidney transplant candidates with high allo-sensitization scores. American Kidney Fund
- Full clinical trials (NKF update, Aug 2025). Nationwide enrollment began for prospective, single-arm studies targeting 60 participants across six centers, with 12-month graft-survival as the primary endpoint. National Kidney Foundation
Internal link: Curious how xenografts could offset dialysis economics? Our deep-dive on dialysis cost drivers breaks it down.
Safety, Ethics, and Public Perception
Imagine the surgical lights fading as Mr Slayman was wheeled from the OR – family hopeful, surgeons exhilarated, ethicists already arguing on X (PKA Twitter). This scene captures the polarity of the pig kidney transplant conversation. On one side, the promise of a readily-available organ; on the other, visceral unease about crossing a species line.
A 2025 U.S. patient-attitude survey found barely 13 % of respondents willing to enroll in a first-in-human xenograft trial. PMC A parallel UK poll echoed the ambivalence: acceptance rises once safety data accumulate, but two-thirds still voice concern about animal welfare and zoonotic risk. The Lancet These worries cannot be summarily dismissed in the modern age, even when human lives are in the balance. Designer pigs live in $75 million biosecure barns, their air showered and their feed irradiated to keep PERV-free status. AP News
Critics argue that “pathogen-free” can drift into “empathy-free” if regulatory inspections slacken. Religious scholars debate whether porcine DNA inside a human violates kosher or halal law; transplant chaplains counter with lived stories of dialysis demise. The ethics remain debatable, but the rising death toll from organ shortage keeps the main issues brutally grounded.
Regulatory & Supply-Chain Hurdles
In late-September 2025 the FDA released an updated Cellular & Gene Therapy Guidance Agenda that, for the first time, lists xenotransplantation as a specific high-priority workstream. U.S. Food and Drug Administration Sponsors must demonstrate:
- Source-animal traceability from embryo to operating room;
- Real-time PERV monitoring with release-criteria algorithms;
- Red-flag registries for recipients and close contacts extending 30 years.
Those requirements drive cost. Revivicor’s pathogen-free farm now logs each pig’s microbiome profile – an SOP that adds roughly US $15 000 to every future pig kidney transplant before the organ leaves the gate. Scaling that to 25 000 grafts a year (today’s U.S. wait-list turnover) means an upstream supply chain comparable in budget to a mid-sized vaccine rollout. Add perfusion devices, CRISPR licensing fees, and xenograft-specific immunosuppressants and the launch price could rival CAR-T therapy.
Logistics bite too: a kidney procured in Virginia must hit a New York OR within six hours, even with normothermic perfusion. That forces hubs near DPF farms, charter flights on demand, and transplant centers willing to re-engineer call schedules. Until payers see long-term actuarial savings, most programs will move cautiously before authorizing payment for human recipients of pig transplant kidneys.
Clinical Impact for CKD Patients
Still, the human calculus is stark. Medicare projects US $273.82 per hemodialysis session in 2025, or roughly US $90 000 per beneficiary each year—not counting hospitalizations. Centers for Medicare & Medicaid Services With rates slated to climb to US $281 in 2026, Centers for Medicare & Medicaid Services (1) every durable xenograft that frees a patient from the machine pays for itself within three to five years, even at a headline price north of US $300 000.
Early compassionate-use data hint at more than cost offsets. Recipients describe “waking up without the dialysis fog,” normalizing phosphorus within days, and planning road trips impossible under thrice-weekly chair time. But access could mirror existing transplant disparities: rural and minority patients already face longer wait-times and fewer referrals; xenograft rollouts risk deepening that divide if high-volume centers charge concierge-style fees.
For now, nephrologists should prep patients with level-headed counseling: a pig kidney transplant is not yet a ticket off the wait-list, but it is no longer science fiction. Encourage potential candidates, especially those with high PRA or multiple failed grafts, to follow trial openings and consider registry enrollment.
Timeline to Mainstream Adoption
2025 – 2027 · “Pioneer Phase.”
With Mr Rick Slayman’s historic pig kidney transplant at Massachusetts General Hospital (MGH) and Towana Looney’s 130-day run at NYU, the field crossed the safety threshold from brain-dead models to conscious recipients. Massachusetts General Hospital(2) FDA reviewers responded by adding xenotransplantation to their high-priority agenda and re-issuing guidance that formalized pathogen-free sourcing and 30-year recipient surveillance. U.S. Food and Drug Administration Over the next 24 months, phase-I “compassionate allotment” trials (≈60 patients) will probe thrombosis, delayed rejection, and immunosuppression load-balancing.
2028 – 2030 · “Scaling Phase.”
If one-year graft-survival tops 70 % roughly par with marginal deceased-donor kidneys, CMS has signaled a willingness to bundle the procedure under the ESRD Prospective Payment System (PPS). The math is straightforward: the 2025 base dialysis rate is $273.82 per session and projected to rise to $281.06 in 2026. Centers for Medicare & Medicaid Services(2) A durable xenograft that liberates a patient from thrice-weekly chair time pays back its upfront cost within five years, even at CAR-T-level launch pricing. Hospitals that already run paired-kidney exchange algorithms could expand to include xenograft slots, smoothing OR schedules and lowering organ-logistics overhead.
2031 – 2035 · “Mainstream Phase.”
By the early 2030s, analysts expect supply-chain kinks with biosecure herds, charter flights, perfusion pumps to stabilize. Modeling studies presented at ASN Kidney Week 2025 predict that once annual production tops 25 000 grafts, unit cost drops below living-donor procurement. At that inflection point, most large U.S. centers will adopt pig kidney transplant programs; smaller hospitals will refer. Public sentiment is already inching forward: a 2025 UK/US survey found that acceptance climbs from 13 % to nearly 50 % once safety data exceed six months. The Lancet If rejection-free survival pushes past two years, actuarial tables suggest insurers will green-light routine coverage.
Take-Home Points & Next Steps
- Not science fiction anymore. Three first-in-human successes prove surgical feasibility and short-term function.
- Regulation is catching up. FDA’s 2025 guidance lays a clear IND path; expect multi-center phase-II trials by late 2026.
- Economics favor adoption. Escalating dialysis PPS rates make a successful pig kidney transplant cost-effective within half a decade.
- Equity must stay front-of-mind. Rural and minority CKD patients already trail in referral rates; providers should track xenograft trial openings and advocate early.
- Stay informed. Follow works cited links as this article is evidence based. Join naturenal.com e-mail subscriber list and return back to this page for updates.
Works Cited
- Donate Life America. National Donate Life Month 2025: Donation & Transplantation Statistics. 2025. Donate Life America
- Mass General Hospital. World’s First Genetically-Edited Pig Kidney Transplant into Living Recipient. Press release, Mar 21 2024.Massachusetts General Hospital
- NYU Langone Health. Pig Kidney Recipient Returns Home After Transplant Breakthrough. Feb 25 2025.NYU Langone Health
- Science. Longest human transplant of pig kidney fails. Apr 11 2025.Science
- FDA. Xenotransplantation Guidances. Updated Jun 17 2025.U.S. Food and Drug Administration
- CMS. CY 2025 ESRD PPS Base Rate. May 29 2025.Centers for Medicare & Medicaid Services
- CMS. CY 2026 ESRD PPS Proposed Rule. Jun 30 2025.Centers for Medicare & Medicaid Services
- Al-Haboubi M et al. Public views on xenotransplantation from the first clinical successes. The Lancet. 2025.The Lancet