Vascular Access in Hemodialysis and Why a Fistula May Be Your Best Choice.
Vascular access is the lifeline of hemodialysis. Without a reliable way to circulate blood between the body and the dialysis machine, the treatment simply cannot occur. Choosing, creating, and caring for a vascular access point is one of the most critical decisions in managing end-stage kidney disease (ESKD). This post explores the three main types of access, their pros and cons, and how to optimize long-term outcomes.
Why Vascular Access Matters
Hemodialysis removes toxins, excess fluid, and waste products from the blood. To do this, blood must travel from the patient to the machine and back at a high flow rate—typically 300 to 500 mL/min. This requires a durable and efficient connection to the bloodstream. The type of access in use has important implications for morbidity (complications) and mortality (risk of death) in ESKD.
The type of vascular access chosen affects:
- Risk of infection
- Functionality and reliability
- Longevity and reusability
- Hospitalization and complication rates
Getting the access type right can significantly impact a patient’s quality of life and treatment success.
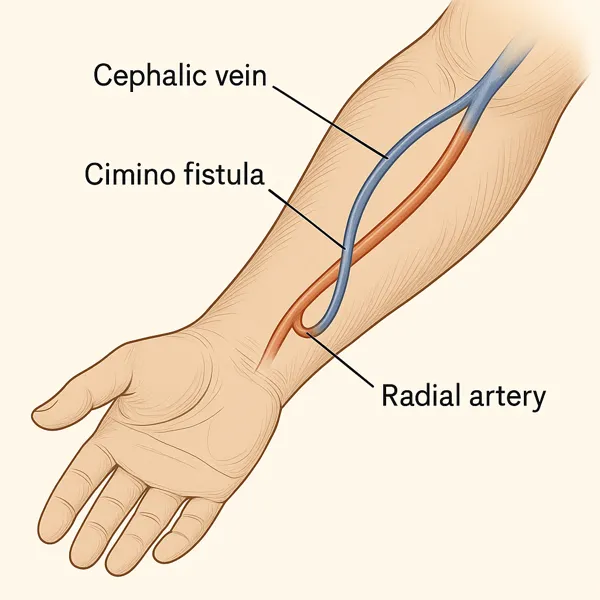
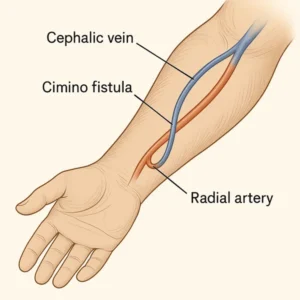
Arteriovenous Fistula (AVF): The Gold Standard
An arteriovenous fistula (AVF) is a surgical connection between an artery and a vein, usually in the arm. This connection causes the vein to thicken and enlarge over time, making it easier to insert dialysis needles and sustain high blood flow. It is created exclusively out of your own tissues with no foreign bodies or synthetic material left behind (with the exception of suture materials and staples in some cases).
Advantages:
- Lowest infection rate of all access types
- Longest lifespan (often years with proper care)
- Lower clotting risk
Challenges:
- Requires time to mature (4–12 weeks, sometimes longer)
- Not suitable for all patients, especially those with small or diseased vessels
- May fail to mature and need surgical revision
Despite the waiting period, AVFs are generally preferred and recommended by clinical guidelines like NKF-KDOQI and KDIGO.
Arteriovenous Graft (AVG): The Second Option
If a patient’s veins aren’t suitable for an AVF, an arteriovenous graft (AVG) may be placed. This involves surgically implanting a synthetic tube between an artery and a vein.
Advantages:
- Can be used sooner than a fistula (often within 2–4 weeks)
- Easier to place in patients with poor vein anatomy
Drawbacks:
- Higher risk of infection and clotting compared to AVFs
- Shorter lifespan
- May require frequent interventions like angioplasty or thrombectomy
AVGs serve as a viable alternative when fistula creation isn’t possible, but they demand more intensive monitoring and maintenance.
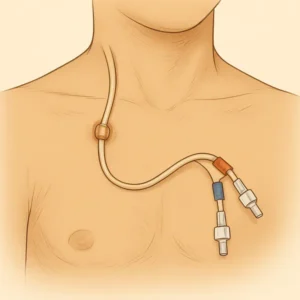
Central Venous Catheters (CVC): A Temporary Lifeline
A central venous catheter (CVC) is a plastic tube inserted into a large central vein, often in the neck or chest. It’s the fastest way to initiate dialysis and is typically used in emergency or short-term situations.
Advantages:
- Immediate use possible
- No need for vessel maturation
- Can be placed bedside
Serious Risks:
- Highest infection risk of all access types
- Prone to clotting and malfunction
- Can cause narrowing (stenosis) of central veins
CVCs are not ideal for long-term dialysis. They are best viewed as a bridge while waiting for a fistula or graft to mature.
Planning Ahead: Why Early Referral Matters
One of the biggest predictors of successful vascular access is timing. Creating an AVF or AVG well before dialysis is needed allows time for healing and maturation. Early nephrology referral is key.
After learning about dialysis modality options, ask your nephrologist when to anticipate access planning:
- Based on my selection of modality do I need to get an access placed soon?
- Am I a candidate for a fistula or peritoneal catheter access?
- Should I see a vascular surgeon?
Patients with advanced CKD (eGFR <20 mL/min/1.73m²) should start access planning—even if dialysis isn’t needed yet.
Care and Maintenance of Your Access
Protecting your vascular access is critical. Here’s how:
- Inspect daily: Look for redness, swelling, or signs of infection
- Feel the thrill: A buzzing sensation indicates proper blood flow in a fistula or graft
- Avoid blood draws and BP: Never allow IVs or blood pressure cuffs on your access arm
- Keep it clean and dry: Especially with catheters
Report any pain, temperature changes, or changes in flow to your dialysis team immediately.
Innovations and Alternatives

Some patients may benefit from newer technologies:
- Endovascular AVFs: Created using catheter-based techniques without open surgery
- HeRO grafts: Designed for patients with central vein stenosis
- Peritoneal dialysis: May be a better option in those with poor vascular access options (see our post on dialysis modality options)
Always explore all your options in collaboration with your care team. Read more about dialysis modality selection.
The Takeaway
Vascular access isn’t just a medical procedure—it’s a long-term investment in your dialysis journey. Understanding the types, risks, and best practices can empower you to make the right choice and advocate for proper care.
If you’re approaching dialysis, don’t wait. Early planning, informed decisions, and active involvement can improve outcomes and preserve independence.
Read more about the benefits of an arterio-venous fistula and the impact of access education here: Fistula First Initiative
Internal Links
References
- Lok CE, et al. KDOQI Clinical Practice Guidelines for Vascular Access: 2019 Update. Am J Kidney Dis. 2020;75(4 Suppl 2):S1–S164.
- Vachharajani TJ, et al. Vascular Access Choices and Their Relation to Outcomes in Dialysis. Clin J Am Soc Nephrol. 2018;13(6):962–969.