The Gut-Kidney Axis: 3 Emerging Therapies for CKD and 1 Cautionary Update.
Introduction
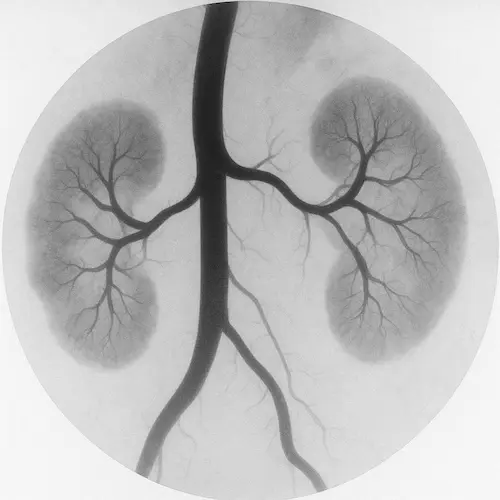
Most people don’t connect the gut and the kidneys — but research is rapidly changing that view. Scientists now describe the gut-kidney axis, the idea that intestinal health and microbial balance can directly shape kidney outcomes. In the past five years, the gut-kidney axis has moved from theory to clinical trials, with drugs, supplements, and targeted therapies showing real-world impact.
Diet has long been identified as a key element of chronic kidney disease management to help sustain residual renal function over time. For patients and families, therapies are being developed to further exploit this relationship, signaling a future where treatment for kidney disease may involve modulating the gut as much as protecting the kidneys themselves. In this article, we will review three promising therapies linked to the gut-kidney axis – and one cautionary example that reminds us the connection can sometimes create harm.
Read more about the importance of diet in CKD. Get a free CKD-DASH diet download by joining the Naturenal email list.
Lubiprostone : A Constipation Drug with Gut-Kidney Axis Potential
Lubiprostone has been prescribed for years as a treatment for chronic constipation. It works by activating chloride channels in the intestine, increasing intestinal fluid and promoting regular bowel movements.
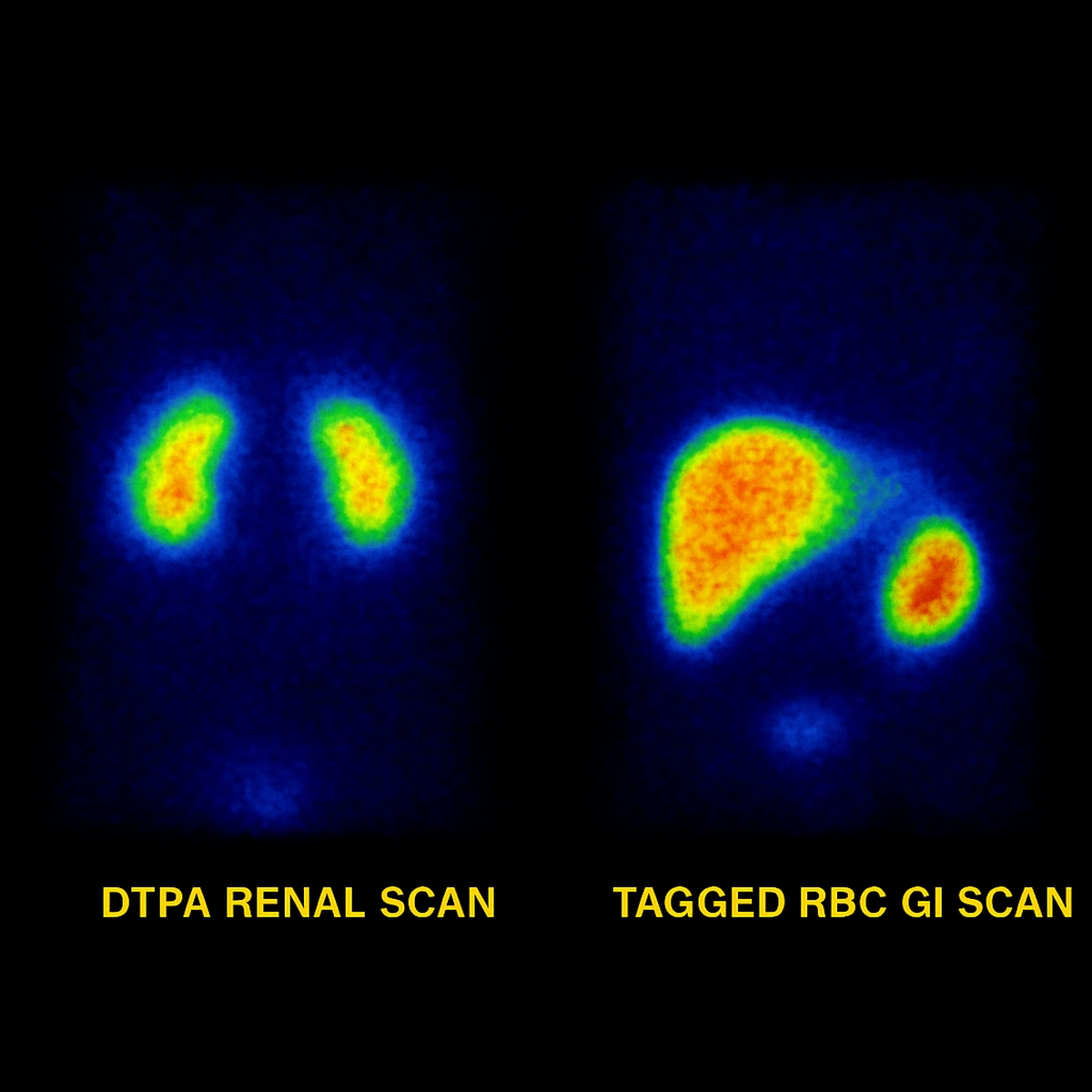
But new evidence suggests lubiprostone may also protect kidney function through the gut–kidney axis. The LUBI-CKD trial in Japan found that patients with chronic kidney disease who took lubiprostone experienced a slower decline in estimated glomerular filtration rate (eGFR) compared to placebo.
The proposed mechanism is striking: lubiprostone boosted levels of spermidine, a compound produced by gut microbes. Spermidine supports mitochondrial health, reduces oxidative stress, and promotes cellular repair – all pathways important in slowing CKD progression.
Patient perspective: If confirmed in larger studies, lubiprostone could be repurposed as a dual-action therapy that relieves constipation and protects kidneys via the gut-kidney axis. For now, its kidney-protective role is investigational and mostly studied in Japan.
Renadyl : A Probiotic That Introduced Patients to the Gut-Kidney Axis
Before prescription drugs took the spotlight, researchers and patients turned to probiotics as a way to influence kidney health. Renadyl is one of the most recognized formulations, combining Streptococcus thermophilus, Lactobacillus acidophilus, and Bifidobacterium longum. The goal is to metabolize toxins in the gut before they reach the kidneys.
Pilot studies showed small decreases in uremic toxins such as indoxyl sulfate and p-cresyl sulfate. However, larger randomized trials have not proven whether Renadyl improves kidney outcomes like eGFR.
Why it matters for the gut-kidney axis: Renadyl may not be a definitive therapy, but it helped shape the idea that gut microbes play a role in CKD. For patients, it remains a supplement some explore under physician supervision, with the understanding that evidence remains limited.
Tarpeyo : Gut-Kidney Axis Immunotherapy for IgA Nephropathy
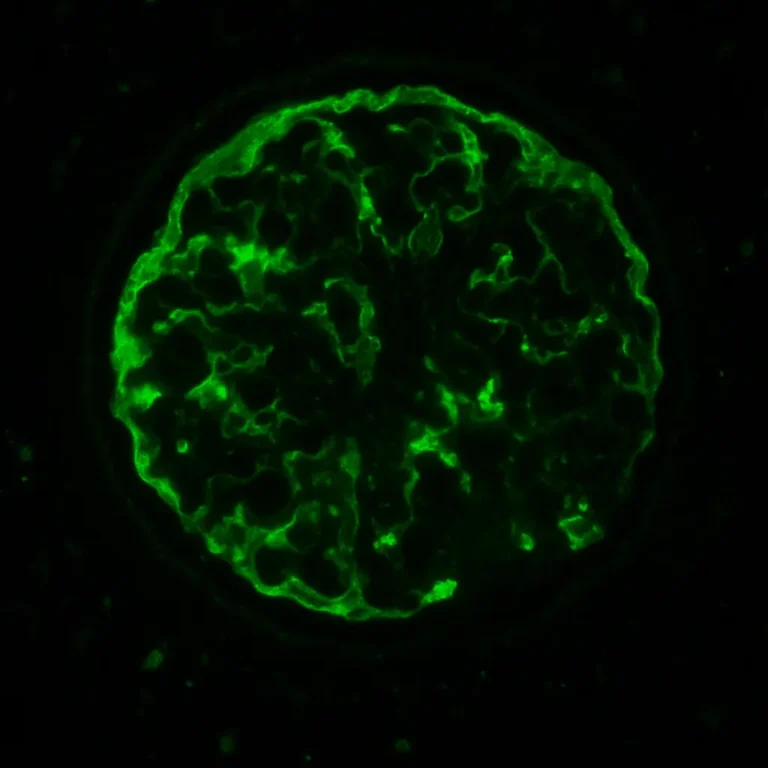
The gut-kidney axis is not only about microbes – it also involves the immune system. Tarpeyo (targeted-release budesonide) is an FDA-approved therapy for IgA nephropathy, a specific type of chronic kidney disease where abnormal immune responses lead to kidney injury.
Tarpeyo delivers budesonide directly to the distal ileum, a site of immune activation in IgA nephropathy. By calming the gut mucosal immune system, it helps lower proteinuria which is known to slow kidney damage in this disorder.
Patient perspective: For IgAN patients, Tarpeyo represents a major step forward. It proves that gut-targeted delivery can meaningfully alter kidney outcomes, underscoring the reach of the gut–kidney axis beyond microbial metabolism into immunology.
Proton Pump Inhibitors : A Gut Drug That Shows the Risk Side of the Gut-Kidney Axis
The gut–kidney axis does not always help. Sometimes gut therapies harm kidneys. Proton pump inhibitors (PPIs), among the most prescribed drugs worldwide, are used for reflux and ulcers. They may be unavoidable in certain GI disorders like Barrett’s esophagus. But long-term use has been linked to a higher risk of chronic kidney disease.
Mechanisms may include:
- Microbiome disruption from acid suppression.
- Magnesium deficiency that stresses kidney function.
- Interstitial nephritis, an uncommon but serious inflammatory reaction.
Patient perspective: PPIs remain safe for many when used appropriately. But nephrologists recommend the lowest effective dose and shortest necessary course. This caution highlights that the gut-kidney axis can cut both ways – helpful at times, harmful at others.
The Future of Gut-Kidney Axis Therapies
Research on the gut–kidney axis is expanding in several directions:
- Prebiotics and dietary fiber: Trials are testing whether added fiber can reduce toxin production in the gut and slow CKD progression.
- Next-generation probiotics and postbiotics: Instead of broad mixtures, scientists are isolating targeted strains and microbial products that may offer more predictable kidney benefits, similar to the science behind Renadyl.
- GLP-1 receptor agonists for NASH: The recent FDA approval of a GLP-1 drug for nonalcoholic steatohepatitis (NASH) highlights how therapies with evolving kidney benefit can have multisystem benefits. These drugs improve weight, insulin sensitivity, and inflammation – all linked to CKD outcomes.
- SGLT2 inhibitors and fatty liver disease: Clinical trials and meta-analyses show that SGLT2 inhibitors not only lower blood glucose and protect kidneys, but also improve liver fat and enzyme levels in NAFLD and NASH. These dual effects strengthen their role in the broader gastrointestinal-kidney connection.
Takeaway: The gut-kidney axis is now central to drug development, FDA approvals, and nephrology research. Patients should not self-experiment, but asking a nephrologist how gut health connects to kidney care is becoming increasingly relevant.
Conclusion
The gut-kidney axis is reshaping nephrology. Lubiprostone shows how gut-driven metabolites may protect kidney function. Renadyl introduced patients to probiotics as part of the gut-kidney axis story. Tarpeyo proves that targeted gut immunotherapy can change outcomes in IgA nephropathy. And proton pump inhibitors serve as a warning that gut therapies can sometimes damage kidneys.
Looking ahead, incretin-based drugs and SGLT2 inhibitors show that therapies aimed at the gut-liver-metabolic system can indirectly safeguard kidneys as well. The gut-kidney axis is no longer theoretical – it is a therapeutic frontier blending microbiology, immunology, and patient care.
Works Cited
- Yamamoto T, et al. Phase II trial of lubiprostone in chronic kidney disease. Bioengineer. 2025.
- Ranganathan N, et al. Pilot study of Renadyl in CKD patients. Transl Med. 2018.
- FDA Press Release. Tarpeyo approval for IgA nephropathy. 2021.
- Lazarus B, et al. Proton pump inhibitor use and risk of CKD. JAMA Intern Med. 2016.
- KDIGO CKD Guidelines, 2022.
- Androutsakos T, et al. SGLT2 inhibitors and non-alcoholic fatty liver disease: a review. World J Hepatol. 2022.
- Wei Q, et al. Efficacy of SGLT2 inhibitors in NAFLD: meta-analysis of RCTs. Front Endocrinol. 2021.
- Lin S, et al. Effect of dapagliflozin on MAFLD. BMJ. 2025.
- The Gut–Kidney Axis in Chronic Kidney Diseases” – K. Tsuji et al., 2024.