Peritoneal Dialysis Adequacy – The Key to Determining the Most Efficient Prescription
What Does Peritoneal Dialysis Adequacy Actually Mean?
If you’re doing peritoneal dialysis (PD), you may have heard your care team say that your treatment is “adequate.” But what does peritoneal dialysis adequacy really mean? Is it a measure of how well you feel, how much fluid you’re removing, or how your labs look?
In clinical terms, peritoneal dialysis adequacy refers to whether your PD is removing enough waste and excess fluid to meet established safety goals. These goals are designed to reduce the risk of complications and to support your quality of life over the long term. Dialysis doesn’t aim for perfection—it aims to get you “enough” clearance to stay stable, comfortable, and well.
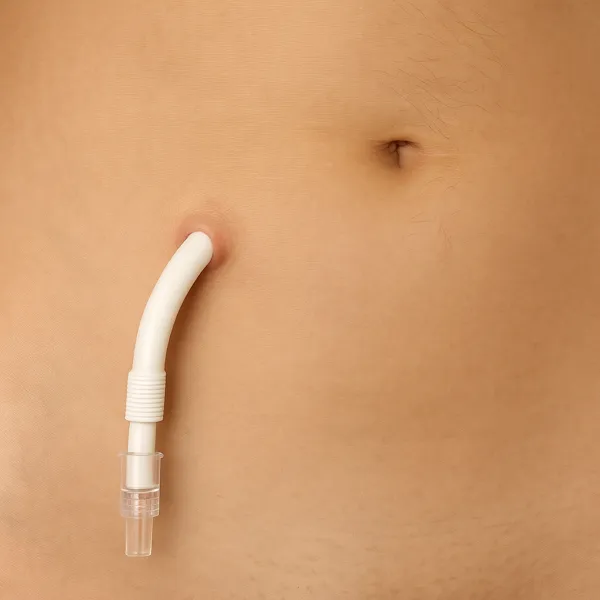
PD works by filling your abdominal cavity with a special solution called dialysate. This fluid pulls waste and extra water from your bloodstream through your peritoneal membrane. After a dwell period, the fluid drains out—and takes the toxins with it. This process repeats several times each day or overnight, depending on your setup.
Adequacy helps your team evaluate whether this system is doing its job. But it’s not just about numbers—it’s also about how you feel and whether your treatment matches your body’s changing needs.
The Main Tool: Weekly Kt/V
To determine your individualized peritoneal dialysis adequacy, your care team uses a measurement called Kt/V. It may sound technical, but its purpose is straightforward: it estimates how much waste is being cleared from your body each week through dialysis and any remaining kidney function you may have.
Here’s a breakdown:
– K stands for the rate of clearance—how efficiently toxins are removed
– t is time—how long dialysis is performed
– V is the volume of distribution, which represents the total body water you’re cleaning
In PD, this is measured on a weekly basis because your treatment is continuous, not in isolated sessions like hemodialysis. The minimum target for peritoneal dialysis adequacy is a weekly Kt/V of 1.7 or higher. That number includes both the waste cleared by your dialysis exchanges and what your kidneys still remove on their own.
If your Kt/V is too low, it doesn’t necessarily mean you’ve failed—it just means it’s time to consider adjustments. Your prescription can often be modified to improve clearance without sacrificing comfort or lifestyle.
Your Kidneys Still Matter: Protecting Residual Function
Even after starting dialysis, many people are surprised to learn that their own kidneys might still be doing part of the work. This is called residual renal function—and it’s one of the most valuable assets you have. Residual function helps remove waste and fluids between exchanges, supports better blood pressure control, and improves outcomes. In fact, studies show that patients with some preserved kidney function tend to feel better and live longer on dialysis.
Your residual function contributes to your peritoneal dialysis adequacy score, which means it directly affects whether your treatment is considered sufficient. For that reason, protecting what’s left of your kidney function is a top priority.
Here’s how you can help:
– Collect every drop during your 24-hour urine test. This is the only way your team can accurately calculate how much clearance your kidneys are still providing.
– Avoid nephrotoxic drugs, especially NSAIDs like ibuprofen and naproxen, which can accelerate loss of function.
– Control blood sugar and blood pressure, as poorly managed diabetes or hypertension can damage what’s left.
– Take prescribed diuretics as directed—these may help you continue to make urine and stay drier between exchanges.
Residual function won’t last forever, but delaying its decline buys you time, flexibility, and better quality of life on PD.

Adjusting the Prescription: Why PD Isn’t One-Size-Fits-All
Peritoneal dialysis is one of the most customizable forms of kidney replacement therapy. Unlike in-center hemodialysis, which typically follows a rigid schedule and standardized dose, PD offers a high degree of flexibility. That flexibility isn’t just a convenience—it’s central to achieving and maintaining peritoneal dialysis adequacy over time.
Peritoneal dialysis adequacy, as you’ve learned, is about clearing enough waste and fluid to meet safety targets. But those targets don’t live in a vacuum. Your body changes. Your residual kidney function may decline. Your lifestyle may evolve. That’s why the PD prescription needs to be dynamic—something that’s reviewed and revised as needed.
Your prescription includes several adjustable components:
1. Dwell Volume
This is the amount of dialysate infused into your abdomen during each cycle. A larger dwell volume can increase the surface area for exchange and may improve solute clearance. However, too much fluid can cause abdominal discomfort, difficulty breathing, or even impair appetite by pressing on the stomach.
2. Number of Exchanges
If your residual kidney function is good, you might start PD on an incremental schedule—just a few exchanges per day or night. Over time, as kidney function declines, your team may increase the number of cycles to maintain total clearance. For example, a patient might go from five nightly exchanges to six, or add a midday dwell to their regimen. The most impactful changes to peritoneal dialysis adequacy are achieved through adjustments in the total volume of PD fluid prescribed daily.
3. Dwell Time
Not all patients absorb and clear toxins at the same rate. The characteristics of the peritoneal membrane are variable and can change over time. The peritoneal equilibration test (PET) helps categorize you as a slow, average, or fast transporter. Slow transporters often need longer dwell times, while fast transporters may benefit from shorter cycles to avoid reabsorption of toxins and glucose. The PET result is used to personalize your dwell durations to maximize efficiency. This is also one of the reasons why peritoneal dialysis adequacy varies between different patients on the same prescription.
4. Dialysate Strength
PD solutions come in varying glucose concentrations—1.5%, 2.5%, and 4.25%. These determine how much water is drawn out of your bloodstream. If you’re fluid overloaded, a higher strength might be used to remove more water. However, stronger glucose solutions can be tough on the peritoneal membrane over time and may raise blood sugar in patients with diabetes.
5. Icodextrin (Extraneal)
This is a starch-based alternative to glucose-based dialysate, used for long dwell periods like daytime dwells in automated PD or overnight dwells in manual CAPD. Icodextrin offers steady fluid removal over extended periods and is especially useful for patients who absorb glucose quickly or struggle with fluid balance.
6. Additional Customizations
Other factors your team may adjust include:
– Fill volume variation on a per-cycle basis
– Cycler programming to match your sleep and wake cycles
– Use of daytime disconnect options to enable mobility
– Consideration of nutritional intake, which affects toxin buildup and fluid needs

These changes are not one-time decisions—they’re part of an ongoing conversation. Regular labs, 24-hour urine collections, symptom reviews, and open communication with your PD nurse or nephrologist help ensure that your current prescription is still meeting your needs.
Maintaining peritoneal dialysis adequacy isn’t just about reaching a number. It’s about adjusting treatment to support how you feel, how you function, and how your health evolves over time.
How Will I Know If My PD Isn’t Enough?
Lab values can tell us a lot—but they don’t tell the whole story. Even if your weekly Kt/V looks acceptable on paper, you might still feel unwell. That’s because peritoneal dialysis adequacy isn’t just a number—it’s a combination of what the data says and how your body responds.
If your treatment isn’t keeping up, you may notice symptoms like:
- – Persistent fatigue, even after a full night’s sleep
- – Loss of appetite or an odd taste in your mouth
- – Swelling, especially in your legs or around the eyes
- – Shortness of breath, particularly when lying down
- – High blood pressure that’s harder to manage
- – Unexplained weight gain, which may reflect fluid buildup
These signs often point to underdialysis, volume overload, or both—even when Kt/V is technically “adequate.” That’s why your symptoms deserve just as much attention as your labs.
Your care team may respond by adjusting your prescription—adding more exchanges, lengthening dwell time, or changing your dialysate concentration. You don’t need to wait for lab results to raise concerns. If something feels off, speak up regardless of your peritoneal dialysis adequacy measures. In PD, timing matters—and small changes can make a big difference.
A Quick Word on Home Hemodialysis (HHD)
If you’re approaching the limits of what peritoneal dialysis can do for you—or if you’re struggling with symptoms despite adjustments—your care team might mention home hemodialysis (HHD). HHD allows for more frequent and individualized treatments that may offer better toxin clearance and fluid management for some patients.
Switching to HHD doesn’t mean PD failed. It simply means your needs have evolved, and another home-based option might serve you better. HHD can often be tailored just like PD, with flexible schedules and fewer dietary restrictions compared to in-center dialysis.
If that conversation comes up, ask how it compares to your current level of peritoneal dialysis adequacy, and whether it aligns with your goals for independence, energy, and long-term well-being.
Learn more in our companion article: Hemodialysis Adequacy – Understanding this Important Value.
You Have a Say in Your PD Plan
Your peritoneal dialysis adequacy is an important measure of wellness on PD. Tailoring an individual care plan isn’t just a medical formula—it’s a partnership. You have the right to understand, question, and help shape your treatment. In fact, the most effective PD plans are often the result of ongoing dialogue between patients and care teams.
If your schedule is disrupted, your sleep affected, or your symptoms return, there are often practical modifications that can be made without compromising your results. For example, longer connection tubing can allow limited movement while using a cycler. Some patients benefit from transfer sets that enable short periods of disconnection. Others find that custom exchange timing helps them manage work, childcare, or travel more comfortably.
None of this is about “noncompliance.” It’s about optimization. Your nephrologist and PD nurse can work with you to maintain peritoneal dialysis adequacy while improving your day-to-day experience. You don’t have to choose between feeling well and living well.
Stay informed. Speak up. Ask questions. PD isn’t one-size-fits-all—and neither is your life. The right plan is the one that supports both your peritoneal dialysis adequacy and your quality-of-life goals.
Works Cited:
- National Kidney Foundation. KDOQI Clinical Practice Guideline for Peritoneal Dialysis Adequacy: 2015 Update.
- Rhee CM, et al. Incremental dialysis: from concept to practice. Am J Kidney Dis. 2017;69(5):767–777. https://doi.org/10.1053/j.ajkd.2016.10.044