Metabolic Stone Diseases: Getting Relief from Recurrent Stones with Noninvasive Strategies
Introduction: Why Metabolic Stone Disease Matters
Kidney stones are among the most common urologic conditions, affecting nearly one in ten adults during their lifetime. While a first stone event is often managed surgically or symptomatically, the deeper issue lies in the metabolic drivers that make recurrence so likely. This is the realm of nephrology: identifying, treating, and preventing metabolic stone disease before it leads to repeated episodes, chronic kidney injury, or loss of renal function.
The importance of prevention cannot be overstated. Roughly 50% of patients who experience one kidney stone will develop another within ten years. Beyond the immediate pain and cost, recurrent stones contribute to chronic kidney disease (CKD), urinary tract infections, and in severe cases, obstructive uropathy leading to acute kidney injury. Recognizing metabolic stone disease as a systemic disorder reframes management: the goal is not simply to have the urologist remove a stone, but to reduce risk factors, protect nephrons, and preserve long-term renal health.
For patients with recurrent metabolic stone disease, a nephrology-based approach provides clarity. It links diet, hydration, comorbidities such as diabetes and hypertension, and pharmacologic therapy into a comprehensive care plan. For clinicians, it demands familiarity with pathophysiology, urine chemistry, and evidence-based interventions. KDIGO and National Kidney Foundation (NKF) guidelines reinforce the importance of structured metabolic evaluation, including 24-hour urine studies, as a cornerstone of effective prevention.
Pathophysiology of Stone Formation
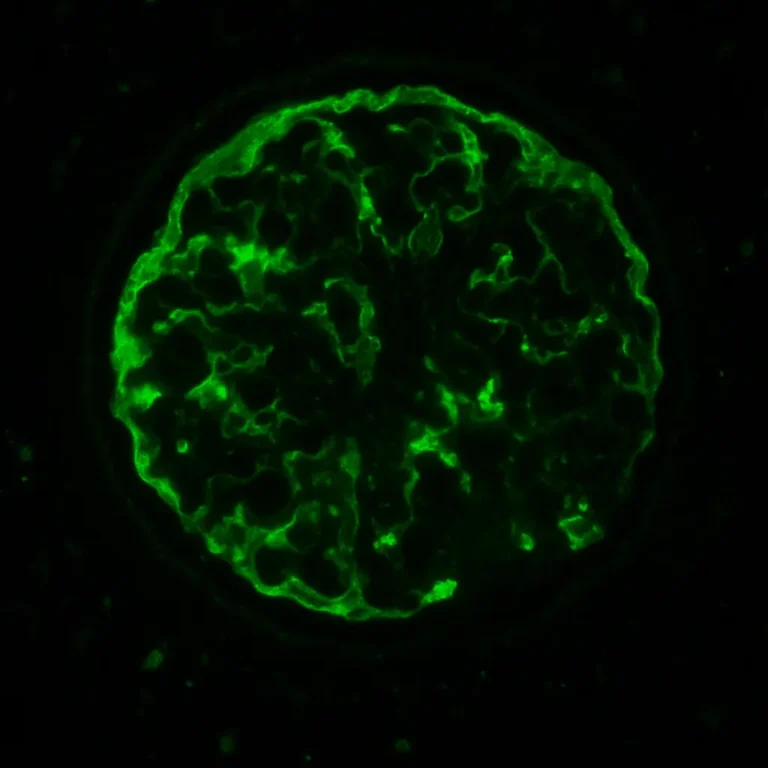
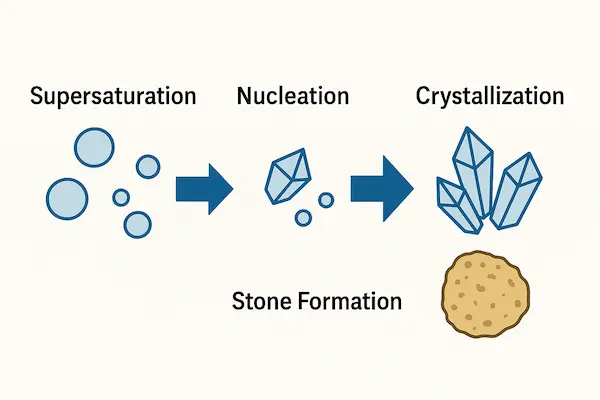
The process of stone formation begins with supersaturation of urinary solutes. When the concentration of calcium, oxalate, uric acid, or cystine exceeds their solubility thresholds, crystals form. It is not pathologic for these molecules to appear in the urine dissolved in solution, but once the concentration reaches a tipping point, the fall out of solution into solid form (nucleation) over which kidney stones develop and aggregate. Supersaturation is influenced not only by solute load but also by urine volume: low fluid intake remains the most consistent risk factor across all stone types. Once nucleation occurs, crystals may grow, aggregate, and anchor within the kidney’s papillae, eventually forming stones large enough to cause obstruction.
Yet supersaturation alone is not the full story. Protective factors normally act as inhibitors, reducing the likelihood that crystals will coalesce. Citrate is the best known: it binds calcium and lowers free ion availability. Magnesium, glycosaminoglycans, and proteins such as nephrocalcin also play inhibitory roles. When these protective factors are deficient, stone formation accelerates.
Metabolic stone disease represents the convergence of these imbalances. Hypercalciuria, hyperoxaluria, hyperuricosuria, and cystinuria are classic examples of measurable biochemical drivers. Secondary contributors include metabolic acidosis, hypocitraturia, and volume depletion. Many systemic conditions — obesity, diabetes, gout, inflammatory bowel disease, bariatric surgery — alter urinary chemistry in ways that heighten stone risk.
Importantly, nephrologists also consider the interaction between CKD and stones. Recurrent nephrolithiasis increases the risk of progressive CKD, while reduced GFR can itself alter solute handling, creating a feedback loop. Albuminuria and hypertension, common in stone formers, further compound renal risk. Understanding these connections helps clinicians move beyond a one-time intervention toward long-term kidney preservation.
In practice, the pathophysiology framework guides evaluation. A patient presenting with calcium oxalate stones, for instance, may have idiopathic hypercalciuria, low urinary citrate, or excessive dietary oxalate intake. Each factor is targetable through diet, pharmacotherapy, or both. Without such an approach, patients remain trapped in the cycle of stone recurrence.
Common Metabolic Stone Disease Types
Understanding the subtypes of metabolic stone disease is crucial for tailoring prevention. While kidney stones may appear as a single problem to patients, the biochemical drivers differ significantly. Nephrologists categorize stones by composition, each with distinct risk factors and interventions.
Calcium oxalate stones
- The most common type, representing ~70–80% of stones.
- Drivers: hypercalciuria, hyperoxaluria, hypocitraturia, or low urine volume.
- Risk amplifiers: high dietary sodium, excessive animal protein, low dietary calcium, or genetic predisposition.
- Management: thiazide diuretics to lower calcium excretion, potassium citrate to restore urinary citrate, and tailored dietary counseling.
Calcium phosphate stones
- More common in women and patients with distal renal tubular acidosis.
- Driven by high urinary pH and calcium excretion.
- May overlap with calcium oxalate stones.
- Management focuses on correcting acid-base balance, reducing sodium intake, and sometimes thiazide diuretic use to manipulate urine chemistries.
Uric acid stones
- Linked to persistently low urine pH (<5.5).
- Associated with obesity, diabetes, gout, and metabolic syndrome.
- Treatment: urine alkalinization with potassium citrate or sodium bicarbonate is highly effective, sometimes with allopurinol if high urine uric acid (hyperuricosuria) is present.
Cystine stones
- Result from the genetic disorder cystinuria.
- Stones recur early and often, requiring lifelong management.
- High fluid intake (often >3–4 L/day), alkalinization, and thiol-binding agents (tiopronin, penicillamine) may be necessary.
Struvite stones
- Formed in association with urease-producing infections.
- Not strictly part of metabolic stone disease, but important in differential management.
- Surgical clearance and infection eradication are priorities, with prevention focused on reducing recurrence risk.
By categorizing stones in this way, nephrologists highlight that prevention is not one-size-fits-all amongst the metabolic stone diseases. Each patient’s stone profile, shaped by metabolic evaluation, directs therapy.
Evaluation in the Nephrology Clinic
The workup of metabolic stone disease aims to uncover modifiable risk factors. A comprehensive evaluation includes history, laboratory testing, and urine analysis, with each step guiding management.

1. Clinical history
- Family history of stones, early onset, or recurrent events point toward genetic risk.
- Lifestyle factors such as low hydration, high salt intake, excess animal protein, or bariatric surgery history are critical.
- Comorbidities including diabetes, gout, obesity, and CKD increase suspicion for metabolic drivers.
2. Laboratory evaluation
- Serum tests: calcium, phosphorus, uric acid, electrolytes, bicarbonate, creatinine, and parathyroid hormone when hypercalcemia is present.
- Renal function: eGFR helps contextualize findings, as reduced GFR alters solute handling.
- CKD staging: important for integrating stone risk with long-term kidney protection.
3. 24-hour urine collection
This remains the gold standard for risk assessment in metabolic stone disease. Measurements typically include:
- Volume (goal >2.0 L/day).
- Calcium, oxalate, citrate, uric acid, sodium, potassium, magnesium, creatinine.
- Urine pH, critical for uric acid and cystine stones.
Results direct individualized therapy: high urinary calcium may justify thiazide use; hypocitraturia suggests potassium citrate; low urine pH warrants alkalinization. Importantly, repeat collections help monitor adherence and therapeutic effect.
4. Imaging follow-up
Low-dose CT and ultrasound provide stone burden assessment, help track recurrence, and guide surgical referrals when needed. In the nephrology clinic, imaging is also used to detect nephrocalcinosis, which signals chronic metabolic disturbance.
5. Risk stratification
Patients with metabolic stone disease presenting with recurrent stones, bilateral disease, family history, or comorbid CKD warrant more intensive monitoring. The presence of albuminuria, hypertension, or progressive eGFR decline should shift management from stone prevention alone to full CKD risk mitigation.
Nephrology evaluation transforms stone care from episodic treatment into proactive prevention against progressive metabolic stone disease. Patients who once cycled through painful ER visits and procedures gain a roadmap: measurable targets, follow-up labs, and a long-term plan for kidney preservation.
Management Strategies by Stone Category
Effective management of metabolic stone disease requires aligning therapy with stone composition and biochemical drivers. While general principles apply to all patients—hydration, dietary optimization, and risk factor control—specific strategies vary by subtype.
Calcium oxalate stones
- Lifestyle and diet: Encourage high fluid intake targeting urine output >2–2.5 L/day. Limit sodium (<2 g/day) to reduce calcium excretion, and maintain normal dietary calcium (not restriction) to bind oxalate in the gut. Excessive animal protein should be avoided, and oxalate-rich foods (spinach, nuts, chocolate) moderated.
- Pharmacologic therapy: Thiazide diuretics reduce hypercalciuria by enhancing distal tubular calcium reabsorption. Potassium citrate raises urinary citrate and corrects acidosis.
- Monitoring: Repeat 24-hour urine studies at 6–12 months to evaluate response.
Calcium phosphate stones
- Lifestyle: Similar to calcium oxalate strategies, but avoid excess alkali intake, as high urine pH promotes phosphate crystallization.
- Pharmacologic therapy: Address underlying distal renal tubular acidosis when present. Sodium restriction and thiazides may reduce stone recurrence.
Uric acid stones
- Lifestyle: Hydration plus urine alkalinization is critical. Diet should limit purine-rich foods (organ meats, shellfish, red meats) and fructose-containing beverages.
- Pharmacologic therapy: Potassium citrate or sodium bicarbonate can raise urine pH to >6.0, dissolving uric acid stones and preventing new ones. Allopurinol is reserved for patients with persistent hyperuricosuria despite dietary modification.
Cystine stones
- Lifestyle: Aggressive hydration to achieve urine output >3–4 L/day. Patients may need overnight fluid infusion in severe cases.
- Pharmacologic therapy: Urine alkalinization is key; thiol-binding agents such as tiopronin or penicillamine are considered when conservative measures fail.
- Monitoring: Lifelong follow-up is required, often with repeated imaging.
Struvite stones
- Lifestyle and monitoring: Patients require close infectious disease and urology collaboration. Prevention focuses on eradicating infection and monitoring for recurrence.
- Pharmacologic therapy: Urease inhibitors such as acetohydroxamic acid may be considered, though rarely used due to side effects.

Ultimately, management emphasizes not only stone clearance but long-term metabolic balance. Urologists manage acute stone events, and some will also manage the non-surgical issues. Nephrologists do not do surgery or stone related procedures but do manage recurrence prevention, which is as important as acute therapy, making the difference between episodic surgical care and sustained renal protection.
Prevention and Follow-up in CKD Context
Metabolic stone disease is not an isolated condition—it has direct implications for kidney health over a lifetime. Patients with recurrent stones have a higher risk of chronic kidney disease, driven by repeated obstruction, infection, and tubular injury. Conversely, patients with CKD face altered solute handling that predisposes them to stones, creating a two-way relationship.
1. Long-term monitoring
- Nephrologists track not only stone recurrence but also eGFR trajectory. Even patients with preserved function at baseline require periodic renal panels and urine albumin testing.
- Imaging with ultrasound or low-dose CT at regular intervals helps detect silent stones before they cause obstruction.
2. Integration with CKD care
- Blood pressure control, diabetes management, and cardiovascular risk reduction overlap with stone prevention. For example, limiting sodium lowers both urinary calcium and blood pressure, while dietary modifications may also be needed based on 24-hour urine chemistry results.
- KDIGO guidelines recommend considering the “big picture”: addressing CKD-MBD, anemia, and cardiovascular risk in parallel with management of metabolic stone disease. Not just treating stone risk in a vacuum.
3. Patient education and empowerment
- Patients should be encouraged to bring a structured tracker—documenting eGFR, urine chemistry, and blood pressure—to each clinic visit. This creates continuity between nephrology care, primary care, and lifestyle management.
- Tools such as a food diary, symptom journal, and the Naturenal CKD Tracker can be leveraged to integrate stone prevention into a broader kidney wellness framework.
4. Follow-up labs
- Repeat 24-hour urine collections remain central. Patients often improve after counseling but may relapse into old habits; objective measurement reinforces accountability.
- Medication adherence must also be tracked: thiazide discontinuation, for example, leads to rebound hypercalciuria and recurrent stones.
5. Holistic care
- Preventive care extends to vaccination, bone health, and dietary counseling. For patients with cystinuria or uric acid stones, early genetic or metabolic consultation may be warranted for inheritable metabolic stone disease disorders.
- Lifestyle coaching should emphasize achievable goals: fluid intake tied to daily routines, realistic sodium reduction, and exercise targets.
By framing stones as part of systemic CKD risk, nephrologists elevate the conversation from “treating a stone” to preserving renal function and quality of life. The message for patients is clear: addressing metabolic stone disease today reduces the chance of both recurrent stones and future dialysis dependency.
Conclusion: A Nephrology Roadmap for Metabolic Stone Disease
Kidney stones may begin as an isolated episode, but repeated recurrences point to an underlying metabolic stone disease that demands nephrology involvement. A structured evaluation—history, serum labs, 24-hour urine testing, and imaging—reveals the drivers of stone risk. Management then shifts from episodic procedures to durable prevention: fluid optimization, dietary change, and targeted pharmacologic therapy.
For patients with comorbid CKD, hypertension, diabetes, or cardiovascular disease, prevention strategies align seamlessly with overall renal protection. The same measures that lower stone recurrence—such as reducing sodium, moderating protein intake, and supporting blood pressure control—also help preserve long-term kidney function. By reframing metabolic stone disease as part of systemic renal risk, nephrology provides a roadmap not only to fewer stones, but also to fewer hospitalizations and better quality of life.
When recurrent stones are compromising quality of life and strength of kidney function, clinicians must treat beyond the stone. Patients must modify their diets, increase fluid intake, engage with preventive plans, and optimize urine chemistry to help dissolve existing stone and prevent new ones. Together, these steps transform metabolic stone disease care from reactive intervention to proactive kidney wellness.
Patient-Centered Takeaways
- Know your type: Kidney stones differ—calcium, uric acid, cystine, and phosphate stones each require unique prevention.
- Hydrate daily: Aim for >2 liters of urine output per day (3–4 liters for cystine).
- Check your diet: Limit salt, moderate animal protein, and maintain balanced calcium intake.
- Use medicines wisely: Thiazides, potassium citrate, or other targeted therapies may prevent recurrence—ask if they are right for you.
- Track labs and blood pressure: Monitoring trends helps both you and your care team stay ahead.
- Think long-term: Preventing metabolic stone disease protects kidney function and lowers the risk of CKD progression.
Works Cited
- KDIGO Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl. 2012; 3(1).
- KDIGO Clinical Practice Guideline for Kidney Stones. Kidney Int Suppl. 2024 (anticipated updates).
- National Kidney Foundation. Kidney Stones: Your Guide to Prevention and Treatment. https://www.kidney.org/atoz/content/kidneystones
- Pearle MS, Goldfarb DS, Assimos DG, et al. Medical management of kidney stones: AUA guideline. J Urol. 2014;192(2):316–324.
- Curhan GC. Epidemiology of stone disease. Urol Clin North Am. 2007;34(3):287–293.