Chronic Kidney Disease Rise: Beyond the Shocking National Geographic Wake Up Call
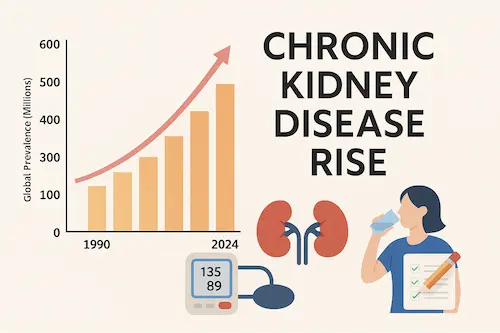
Chronic kidney disease (CKD) has become one of the most pressing – and least recognized – health challenges of our time. On September 3, 2025, National Geographic highlighted this in stark terms: more than 600 million people worldwide are now living with CKD. That chronic kidney disease rise represents a 90 percent increase since 1990, a surge so dramatic that it is reshaping global health priorities.
For people in the United States, the picture is equally sobering. Nearly 35.5 million adults are affected — about one in seven. Even more alarming, the National Kidney Foundation estimates that 9 out of 10 people with CKD don’t know they have it. This “silent epidemic” often progresses unnoticed because kidney damage rarely causes pain or obvious symptoms in its early stages. By the time patients feel sick, kidney function may already be significantly impaired.
Why does this matter? Because CKD is not just a kidney problem. It’s a systemic condition tightly linked to heart disease, diabetes, high blood pressure, and premature death. In fact, most patients with CKD die from cardiovascular complications before ever reaching dialysis or transplantation. That’s the piece that many headlines, including National Geographic’s, gloss over: CKD is not just about kidneys failing, it’s about the entire body being at risk when kidneys are unhealthy.
The rise in chronic kidney disease is not simply a matter of statistics. It’s a wake-up call. The global burden of CKD has grown faster than population expansion, and it reflects both medical progress — people are surviving longer with diabetes and hypertension — and systemic failures, as millions go undiagnosed and untreated until it is too late.
The Chronic Kidney Disease Rise is Alarming
The National Geographic article highlights some of the drivers, but to really understand the chronic kidney disease rise, we need to unpack the full picture. The surge in CKD is the result of multiple overlapping risk factors — some familiar, some less obvious, and some still mysterious.
1. Diabetes and Hypertension
The two biggest culprits are no surprise: diabetes and high blood pressure. Together, they account for the majority of CKD cases worldwide. Elevated blood sugar damages the kidney’s delicate filtration units over time, while uncontrolled hypertension scars blood vessels and reduces kidney perfusion. As global rates of obesity, sedentary lifestyle, and poor dietary habits continue to climb, so too does the prevalence of these root causes.
2. Silent Progression and Late Detection
Unlike heart attacks or strokes, CKD does not announce itself with dramatic symptoms. The kidneys can lose up to 90 percent of function before patients feel ill. That’s why routine screening — simple blood and urine tests — is so essential. Unfortunately, screening is inconsistent, especially in low-resource settings and among patients who don’t see a doctor regularly. The result: late diagnoses, when options are limited.
3. Medication Overuse and Hidden Risks
Everyday drugs can accelerate kidney decline when used improperly. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen are commonly identified as contributing to the chronic kidney disease rise. While safe in short bursts, chronic use increases the risk of kidney injury. Certain antacids and proton pump inhibitors (PPIs) have also been linked to higher CKD risk when taken long-term. These risks rarely make it into public headlines, yet they matter in the story of the chronic kidney disease rise.
4. Environmental and Occupational Stressors
Kidneys are uniquely sensitive to environmental insults. Air pollution, contaminated drinking water, and heavy metal exposure contribute to CKD in many parts of the world. Climate change is now a recognized factor, too: prolonged heat waves increase dehydration risk, stressing kidney filtration and raising the likelihood of long-term injury. Agricultural workers in Central America and South Asia, for instance, are experiencing unusually high rates of chronic kidney disease ris not explained by diabetes or hypertension alone.
5. Healthcare Access and Social Disparities
In the U.S. and abroad, CKD disproportionately affects marginalized populations. Limited access to preventive care, financial barriers, and lack of early detection infrastructure mean many patients only learn they have kidney disease when they present with advanced complications. This is not just a medical issue – it is a reflection of structural inequities in healthcare delivery which obscure the continued chronic kidney disease rise.
6. The Unknowns
Perhaps most unsettling: researchers acknowledge that not all of the chronic kidney disease rise can be explained by traditional risk factors. Some part of the increase remains unexplained, suggesting there are environmental, genetic, or lifestyle influences we have yet to fully recognize.
What the National Geographic Article Missed
The National Geographic report shines a bright light on the sheer scale of the chronic kidney disease rise, but there are critical layers of the story that were left unexplored. These gaps matter because they directly influence how patients, families, and even policymakers perceive the threat of CKD.
The Cardiovascular Link
Most people assume CKD is primarily about dialysis or the possibility of needing a kidney transplant. In reality, the majority of patients with kidney disease will never reach that point because they will die of cardiovascular disease first. When the kidneys are damaged, they can no longer regulate blood pressure, maintain mineral balance, or clear toxins effectively. This accelerates arterial injury, thickens the heart muscle, and fuels strokes, heart attacks, and arrhythmias. Understanding this heart-kidney connection reframes the chronic kidney disease rise as having whole-body impact and not an isolated organ failure.
The Problem of Underdiagnosis
CKD is notorious for being under-recognized. Primary care physicians may prioritize blood pressure, cholesterol, or diabetes management without flagging subtle changes in kidney function. Even when labs show declining eGFR or proteinuria, these may not be discussed until the disease has advanced. The National Geographic article noted the scope of the epidemic, but it did not emphasize another reason for the chronic kidney disease rise is in part due to the systemic blind spot that allows it to progress unchecked.
The Inequity Factor
Kidney disease is not distributed evenly across populations. In the U.S., Black, Hispanic, Native American, and low-income patients are more likely to develop advanced CKD and to progress to kidney failure. Some of this is explained by higher rates of diabetes and hypertension, but social determinants of health – access to fresh food, safe neighborhoods for exercise, affordable medications, and preventive care – play a large role. Failing to highlight this inequity risks treating CKD as an equal-opportunity disease when, in truth, it strikes hardest where systemic disadvantage already exists.
Preventable Hospitalizations
Another piece missing from the media spotlight: the cost of avoidable hospitalizations due to undiagnosed or poorly managed CKD. Patients often present with fluid overload, uncontrolled blood pressure, or electrolyte emergencies that could have been prevented through earlier interventions. This burden weighs not only on patients and families but also on healthcare systems struggling under rising costs.
The chronic kidney disease rise is not just about numbers. It is about missed opportunities – moments when earlier recognition and intervention could have changed the trajectory for millions of people.
New Hope in Kidney Care: Advances Patients Should Know About
Despite the grim statistics surrounding this chronic kidney disease rise, there is genuine reason for optimism. For decades, the story of CKD care seemed to end with dialysis or transplantation. Now, however, a wave of new therapies and research breakthroughs is changing the outlook for patients worldwide.
SGLT2 Inhibitors and GLP-1 Receptor Agonists
One of the most important developments has been the rise of medications originally designed for diabetes management. SGLT2 inhibitors (such as empagliflozin and dapagliflozin) and GLP-1 receptor agonists (such as semaglutide, marketed as Ozempic and Wegovy) are demonstrating powerful kidney-protective effects.
In fact, a major trial of semaglutide in CKD patients was stopped early because the benefits were so striking: patients had lower rates of kidney failure, fewer cardiovascular events, and even improved survival compared to placebo. These findings mark a turning point in nephrology, showing that medications can slow disease progression, not just manage complications. The ongoing increasing rate of chronic kidney disease rise will depend on not only utilization of these agents, but also affordability.
Targeted Therapies for Autoimmune Kidney Disease
For conditions like IgA nephropathy and lupus nephritis – long considered difficult to treat – new biologic therapies are emerging. These drugs target specific pathways in the immune system, offering more precise control than older treatments that relied heavily on steroids and broad immunosuppression. For patients, that means better disease control and fewer side effects.
Polycystic Kidney Disease (PKD) Advances

Autosomal dominant polycystic kidney disease (ADPKD), a common genetic disorder, has historically led to kidney failure in middle age. Today, targeted agents such as tolvaptan are helping slow cyst growth and preserve kidney function for many patients. While not a cure, these therapies buy precious time before advanced disease sets in.
The Push for Early Detection
Equally important is the growing movement toward earlier screening and recognition. Global organizations, including the Kidney Disease: Improving Global Outcomes (KDIGO) initiative, are advocating for routine urine albumin and serum creatinine testing in at-risk populations. By identifying kidney damage earlier, clinicians can implement interventions when they are most effective.
A New Era of Patient Empowerment
Perhaps the most exciting change is not technological but cultural. Patients are gaining more tools to participate actively in their kidney health. Whether it’s tracking blood pressure at home, using digital CKD trackers, or engaging in educational platforms like naturenal.com, patients are no longer passive recipients of a diagnosis – they are partners in delaying progression.
These advances will not reverse the chronic kidney disease rise overnight, but they represent a shift in the narrative. CKD is no longer a disease without options. With the right tools, therapies, and awareness, the trajectory can change.
What You Can Do Right Now to Protect Kidney Health
The observed chronic kidney disease rise is a global issue, but the choices you make today can influence your personal risk. While you cannot control all factors — genetics, environment, or systemic healthcare gaps — you can take concrete steps that reduce the chance of kidney damage or slow progression if CKD is already present.
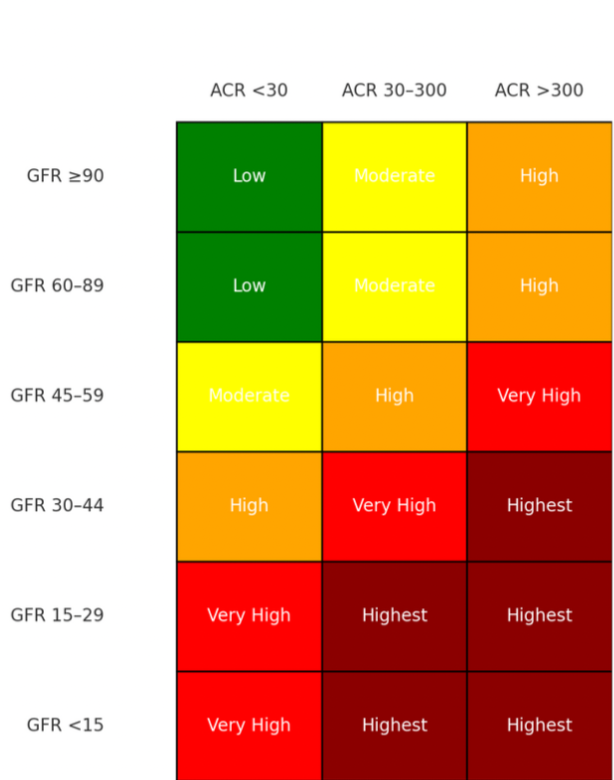
- Know your numbers. Ask your provider about your eGFR (estimated glomerular filtration rate) and urine albumin. These two tests reveal how well your kidneys filter and whether protein is leaking into urine — an early red flag.
- Monitor blood pressure and blood sugar. High blood pressure and diabetes drive the majority of kidney disease. Keeping both within target ranges offers the strongest protection.
- Be careful with over-the-counter drugs. Use NSAIDs (ibuprofen, naproxen) sparingly, and avoid chronic daily use without medical guidance. Talk to your provider before using long-term acid reducers, supplements, or herbal products.
- Stay hydrated and avoid heat stress. Dehydration places a heavy burden on the kidneys. If you work outside or live in a hot climate, make hydration a daily priority.
- Adopt kidney-friendly nutrition. Diets emphasizing fresh fruits, vegetables, moderate protein, and reduced sodium are consistently linked with better kidney outcomes. Avoid overly processed foods and optimize body mass index to control metabolic demand.
At Naturenal we have educational tools and resources to help make these steps easier. Our mission is to empower self-advocacy and understanding – turning scattered numbers into a clear picture you can share with your healthcare team.
The Bottom Line
The National Geographic article brought long-overdue attention to a crisis that has been building for decades: the chronic kidney disease rise is real, steep, and ongoing. More than 600 million people around the world are affected, and most don’t even know it. But statistics don’t tell the whole story.
What the headlines miss is that CKD is not inevitable. New medications, earlier detection strategies, and patient-driven tools are rewriting the outlook. Awareness must be matched with action. By knowing your risks, tracking your health, and working with your care team, you can change the trajectory of kidney disease in your own life.
CKD may be rising worldwide, but your kidneys are in your hands today.
Works Cited
Fairbank, Rachel. “This disease is on the rise—and many people don’t know …” National Geographic. September 3, 2025. Link
Francis, A. et al. “Chronic kidney disease and the global public health agenda.” Nature Reviews Nephrology. 2024. Link
Qi, Q. et al. “Global, regional, and national burden of chronic kidney disease and its associated anemia, 1990–2021.” BMC Nephrology. 2025. Link
National Kidney Foundation. “Chronic Kidney Disease Fact Sheet.” 2025. Link
Centers for Disease Control and Prevention. “Chronic Kidney Disease in the United States.” 2025. Link